Our research – case studies

Could diphtheria become a ‘major global threat’ again as it evolves?
In an international study with the UK and India, researchers have said the impact of COVID-19 on diphtheria vaccination schedules, coupled with a rise in the number of infections, risk the disease once more becoming a major global threat.
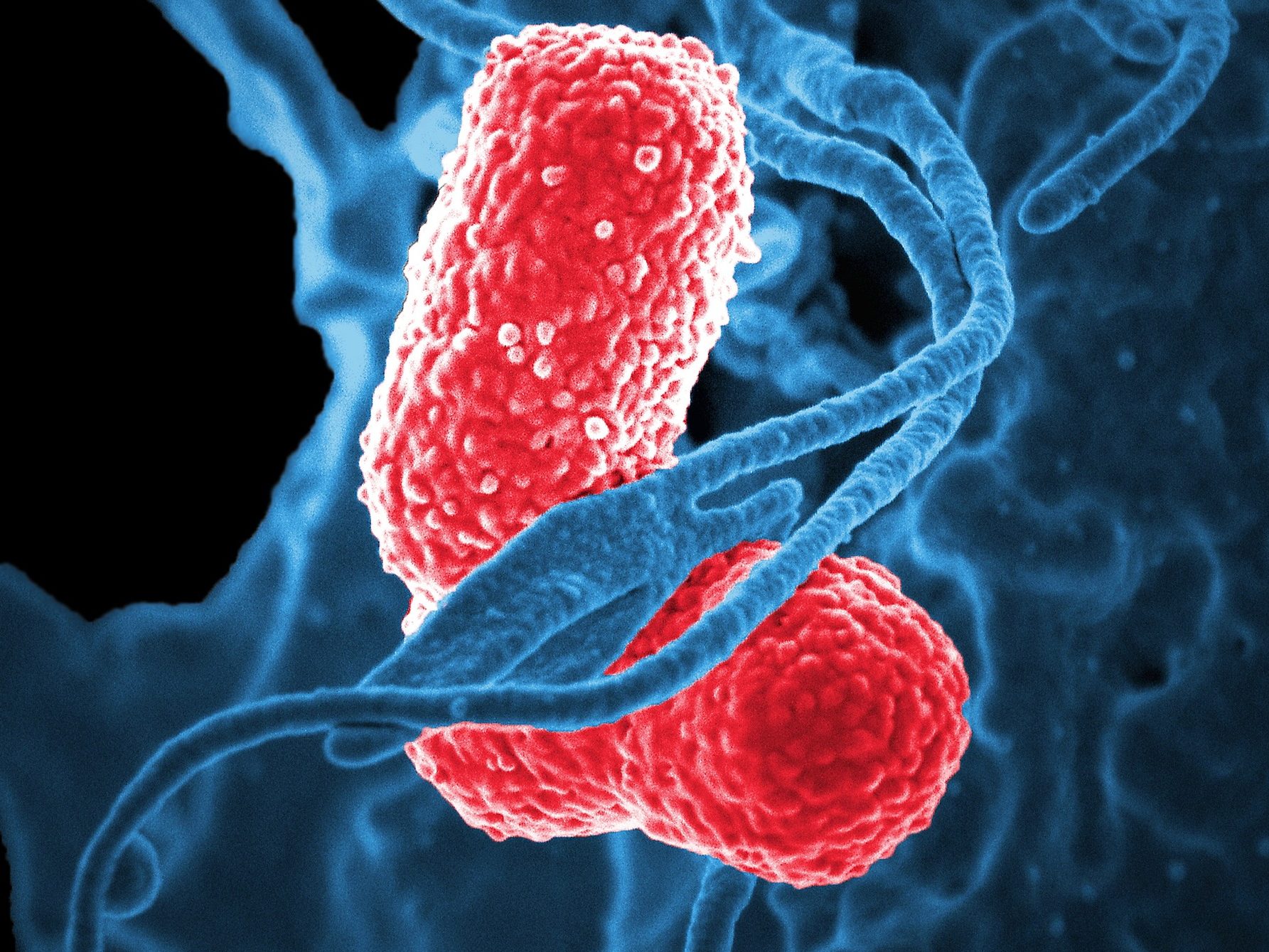
Diphtheria is a highly contagious and potentially fatal infection yet it is easily preventable. Researchers have noticed as it evolves it is becoming resistant to a number of antibiotics.
In high-income countries, babies are vaccinated against infection. However, diphtheria is still problematic in low- and middle-income countries, where the disease can still cause infections in those who are unvaccinated. The disease can be spread through coughs, sneezes or close contact with someone who has been infected. Antibiotics is still the main method to treat the disease.
Researchers analysed the genomes of 61 bacteria isolated from patients and combining these with 441 publicly available genomes, the researchers were able to build a phylogenetic tree – a genetic ‘family tree’ – to see how the infections are related and understand how they spread. They also used this information to assess the presence of antimicrobial resistance (AMR) genes and assess toxin variation.
When the team looked for genes that might identify any resistance to antimicrobials, they found that the average number of AMR genes per genome was increasing each decade. Genomes of bacteria isolated from infections from the most recent decade (2010-19) showed the highest average number of AMR genes per genome, almost four times as many on average than in the next highest decade, the 1990s.
Read the full news story from 8 March 2021.

A DNA test that can identify secondary infections in COVID-19 patients
Researchers have been able to develop a DNA test to quickly identify secondary infections in COVID-19 patients,
Patients who are diagnosed with severe COVID-19 may need mechanical ventilation in order for clinicians to help treat the virus. However, some may be susceptible to secondary bacterial infections.
COVID-19 patients are thought to be more at risk of a secondary infection because of the amount of lung damage from the virus and will spend more time on a ventilator than those without COVID-19. Many of these patients also have a poorly-regulated immune system, where the immune cells damage the organs and also have impaired anti-microbial functions, so trying to diagnose these patients early is vital.
Cambridge researchers have developed a DNA test to identify those who may have developed the secondary infection a lot sooner.
The test uses multiple polymerase chain reaction (PCR) to help detect the DNA of the bacteria within a few hours rather than waiting for it to grow in the lab. The test runs multiple PCR reactions and can simultaneously pick up 52 different pathogens (organism that causes disease), which often infect the lungs of patients in intensive care. At the same time, it can also test for the bacteria which may be resistant to antibiotics.
Often patients have already started to receive antobiotics before the bacteria has had time to grow meaning cultures are often negative. However, the PCR test doesn’t need to viable bacteria to be able to detect it, not only making it a more accurate test and are able to speed up the diagnosis.
This is one of the first times that this technology has been used in routine clinical practice and was approved by Addenbrooke’s hospital in Cambridge.
Read the full story from January 2021
How DNA technologies are helping pneumonia patients fight back
Many patients who are admitted to intensive care show signs of pneumonia, and they are given antibiotics on admission to try and prevent it taking hold. However, this is not always successful and clinicians can find it hard to identify what kind of pneumonia it is.
The antimicrobial resistance team have been working with researchers from Public Health England and clinicians in the Intensive Care Unit at Cambridge University Hospitals to better understand the different types of pneumonia patients may have and to try and identify if they have an infection faster.
To do this, they are using revolutionary DNA-analysis and sequencing technologies that can help them identify exactly which microbes (if any) are contributing to a patient’s pneumonia. Using these technologies, researchers are now able to screen for around 100 kinds of microbes within hours of a sample being taken from the patient and identify which is the best antibiotic to use. Also some patients look like they are infected but are not and these can be quickly picked up. They can also identify how the patient is responding to the infection and help guide better treatment.
Quick identification of the right microbe will enable researchers to select and develop the right antibiotics to fight infection and prevent the disease from developing in vulnerable patients.
Using whole genome sequencing to fight common bugs
Outbreaks of infections of any type within hospitals and communities can put a strain on healthcare services particularly in winter time. This is particularly true if the bugs are resistant to treatment.
Cambridge researchers wanted to investigate how these ‘resistant’ bacteria could be identified faster, so that outbreaks can be reduced and treatments can be given sooner to patients who may be diagnosed with an infection.
Researchers looked at using whole genome sequencing or WGS (a complete set of all the genes of the bacteria including those causing resistance) and examined whether this technique would be an effective mechanism to detect these infectious threats as well as understand their biology and how they are spreading.
Researchers found they were able to identify the bacteria and their resistance patterns (e.g. which antibiotics work and which do not) directly from clinical samples taken from patients, using information gleaned from WGS. They noticed that using WGS gave more accurate information about the microbes and that it provided much better and much more detailed information than normal laboratory methods.
Researchers are continuing to look at ways of improving how these technologies can prevent the spread of infections and improve treatment selection.

