Our research: case studies

Predicting risk of cancer, heart attacks and other diseases using DNA
The human genome (the complete set of genetic information in an individual) has transformed health research, allowing us to uncover the changes in our genetic make-up that make us susceptible or resistant to common diseases.
We can now create scores, called polygenic scores, which quantify risks for more than 100 common diseases. Polygenic scores are driving a new generation of disease risk models which can guide earlier screening, preventative treatment and diagnostics.
Cambridge BRC investigators have been at the forefront of these efforts, particularly for breast/ovarian cancer1 and cardiovascular disease2. Developed together with clinicians and patients, CanRisk is a powerful web-based prediction tool which identifies women at especially high risk of breast and ovarian cancer, and guides preventive actions. Endorsed by NICE in the UK, American Cancer Society and other major bodies, it is used thousands of times daily in more than 90 countries, supporting women, clinicians and genetic counsellors.
CanRisk supports hundreds of thousands of women each year in making decisions about risk reducing medications and surgery (e.g. mastectomy). CanRisk contributes to lower numbers of women diagnosed with cancer, fewer deaths, improved quality of life and reduced costs. A major recent advance of CanRisk has been incorporation of polygenic scores. CanRisk has gained regulatory approval for use as a medical device in the UK and EEA.
Researchers have designed and deployed the world’s main publicly-available resource for polygenic scores, the Polygenic Score Catalog3.
Each polygenic score in the Catalog is annotated with relevant information, including how the score was developed and applied, evaluation of how well they identify people at high risk, and how equitable they are. The team have developed a reporting framework needed for researchers and clinicians to interpret and evaluate polygenic risk scores around the world, and thus promote best practice and translation into clinical care4.
The team are now implementing a prototype patient management system for primary care which uses all our knowledge and tools for polygenic risk scores for early disease detection on 24 million UK individuals.
This will be developed into a fully implemented system usable by clinicians to help make more personalised clinical decisions; bringing the benefits of our research to many underserved and disadvantaged communities.
1 Genetics in Medicine 2019 PMID:30643217
2 PLOS Medicine 2021 PMID:334443
3 Nat Genet 2021 PMID:33692568
4 Nature 2021 PMID:33692554
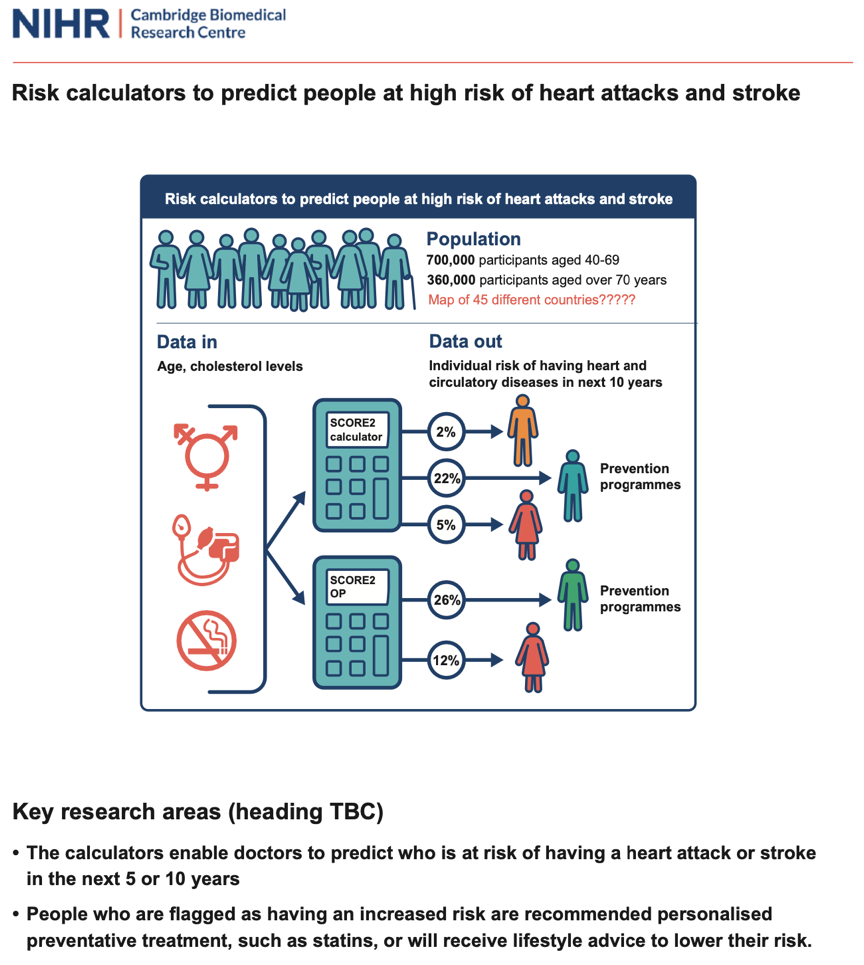
New risk calculators to predict people at high risk of heart attacks and stroke
Cambridge-led working groups and the European Society of Cardiology (ESC) Cardiovascular risk collaboration have developed new risk calculators that can better identify people at high risk of heart and circulatory diseases. These calculators are for use across the UK and Europe1, 2.
The original research focused solely on predicting and preventing mortality, using data from the 1980s. But now more people survive heart attacks and strokes than die from them, especially younger people, so we need to use risk scores of people having non-fatal as well as fatal CVD within 10 years. The SCORE2 calculator was developed using data from nearly 700,000 participants from 45 different studies and has been tailored for use amongst individuals aged 40-69 in the UK and across different European regions.
The SCORE2-OP calculator was developed using data from around 360,000 participants and has been tailored for use amongst older individuals aged over 70 years in the UK and across Europe.
The calculators enable doctors to identify who is at risk of having a heart attack or stroke in the next 5 or 10 years by using known risk factors such as age, sex, cholesterol levels, blood pressure and smoking. They are much-needed upgrades from the previous prediction tools that were developed using data before 1986 and which underestimated the cardiovascular risk in many countries.
The new SCORE2 and SCORE2-OP risk calculators now consider current trends in heart and circulatory diseases, can predict both fatal and non-fatal conditions and are adaptable to countries with different levels of risk.
People who are flagged as having an increased risk can be offered personalised preventative treatment, such as drugs which reduce cholesterol or lifestyle advice to lower their risk.
The tools fit seamlessly into current prevention programmes with substantial real-world impact by improving the early prevention of cardiovascular diseases across the UK and Europe before they strike.
SCORE2 has been adopted by the new European Guidelines on Cardiovascular Disease Prevention in Clinical Practice (August 2021).
What this study adds:
- Improved and up-to-date risk calculators tailored for use amongst individuals from aged 40 years.
- The new calculators take account of current trends in heart and circulatory diseases, can predict both fatal and non-fatal conditions and are adaptable to European countries with different levels of risk.
Impact of the research:
- The calculators enable doctors to predict who is at risk of having a heart attack or stroke in the next 5 or 10 years.
- People flagged at high risk can be offered personalised preventative treatment, such as statins, or lifestyle advice to lower their risk.
- SCORE2 and SOCRE-OP are recommended for use by clinicians across Europe in the newly published (August 2021) European Guidelines on Cardiovascular Disease Prevention in Clinical Practice.
- This research generated major media coverage nationally and globally, including several national UK papers (eg Times, Daily Telegraph, Daily Mirror, Sun, Daily Express) and ~50 regional newspapers.
1European Heart Journal 2021 PMID:3412017
2European Heart Journal 2021 PMID:34120185
Informing healthcare policy with COVID-19 data
The SARS-CoV-2 virus has resulted in more than 235 million cases of COVID-19 and more than 4.8 million deaths worldwide, including approximately 137,000 deaths in the UK (October 2021). Since March 2020, researchers have used health data from a range of sources for examining, modelling and reporting disease trends to inform healthcare and public health policies.
In mid-2020, a new secure data resource covering 54.4 million people – over 96% of the English population – was established for researchers. This work was led by a UK consortium (CVD-COVID-UK) in partnership with NHS Digital. The new resource linked a wide variety of health data, such as those from General Practice records, hospital data and COVID-19 laboratory test and vaccination data. Researchers at the NIHR Cambridge BRC developed data-management strategies, statistical methodologies and computer code1.
The population-wide resource is being used to study individuals with and without health-related problems across all age groups, ethnicities, geographies and socioeconomic settings. The team determined:
- people have higher risks of major cardiovascular and blood clotting diseases for several months after a COVID-19 infection and,
- the COVID-19 Astra-Zeneca vaccine but not the Pfizer vaccine is associated with a small excess risk of rare blood clotting events; but the risk is small compared with the vaccine effect in reducing COVID-19 morbidity and mortality. The results have directly informed health policy decisions by the Chief Medical Officer and Joint Committee on Vaccination and Immunisation.
Researchers played a key role in COVID-19 Genomics UK (COG-UK), the world’s largest SARS-CoV-2 genome sequencing initiative, in partnership with Public Health England and the Wellcome Sanger Institute2. By October 2021 the team sequenced more than 1 million SARS-CoV-2 genomes. COG-UK results guided the Scientific Advisory Group for Emergencies (SAGE) and major policy decisions of the UK government throughout the pandemic, including investigations of outbreaks at local and regional levels across the UK and the importance of different variants3 as well as identification, characterisation and monitoring of “variants of concern”.
For instance, knowing the surge of COVID-19 in Spring 2021 was driven by the Delta variant, prompted stricter travel controls and urgent research into vaccination efficacy against Delta. Once it was clear that one vaccine dose provided less protection against the Delta variant, the population was encouraged to get their second dose earlier.
1BMJ 2021 PMID:33827854
2Lancet Microbe 2020 PMID:32835336
3Lancet ID 2021 PMID:34461056

Screening and Treatment for Abdominal Aortic Aneurysm
Cambridge researchers led a randomised trial to see whether performing ultrasound screening would identify men likely to develop a dangerous AAA, and investigate if early screening can provide long-term benefits.
Abdominal aortic aneurysm (AAA) is an enlargement of the abdominal aorta. It is predominantly found in men over the age of 65, and when it increases in size it can be dangerous and in some cases deadly.
Cambridge researchers led a randomised trial to see whether performing ultrasound screening would identify men likely to develop a dangerous AAA, and investigate if early screening can provide long-term benefits. This was then followed up by a further health economic assessment of AAA screening.
After inviting more than 33,000 men to ultrasound screening and analysing their results against a comparable group not invited, researchers were able to show that population screening of men over 65 could halve the number of deaths from AAA over a 10-year period.
In 2013, the Department of Health in England introduced a national screening programme for men over 65, based on the data from Cambridge researchers which helped shape their policy. A year later Wales, Scotland and Northern Ireland introduced AAA screening for men, and other countries have also adopted the programme.
This national AAA screening programme has saved many lives via early detection and treatment of AAA.

Reviewing the NHS Health Check programme
The NHS Health Check programme was introduced across England in 2009 for people aged 40 and above who do not have known health conditions. People take the checks at their local surgery to find out their risks of developing conditions such as heart disease, stroke and diabetes.
The NHS Health Check programme offers people information on how to reduce their risk and/or early treatment. Many of the recommended lifestyle changes also lower the risk of other diseases, such as cancer and lung disease.
Under the current ‘one size fits all’ guidelines, the checks are available to all apparently healthy people every five years until they reach 75. However, within this group some will be at higher risk of future disease and may benefit from earlier and more frequent health checks – while those at lower risk will need fewer checks.
To identify people with greatest health needs, researchers have been developing methods to use data from electronic health records (which all patients have), including measurements of the “risk factors” that are known to be linked with greater risk of disease. These include smoking, being older, being overweight, and having high blood pressure and high cholesterol.
GPs will be able to use this tool to estimate when individuals should next be invited for an NHS health check. This may help increase the cost-effectiveness of the programme while directly benefiting those at highest risk of future disease.

