PhD Programme for Health Professionals now open for applications
An exciting PhD Programme for Health Professionals has been established in partnership between the Universities of Cambridge and East Anglia and the Wellcome Sanger Institute. From 2022, funding is available for seven Fellowships each year for the next five years.
The scheme is ideally suited to clinical health professionals of the highest calibre, seeking to pursue a successful academic career.
If appropriate, predoctoral research placements in different research groups enable fellows to make an informed choice of supervisor and project, leading to a PhD.
In addition, the programme offers bespoke training and mentoring for a successful research experience, and guidance postdoctorally. Many graduates of the previous Clinical PhD Programme have continued in an academic pathway, gaining higher research fellowships, and achieving academic faculty positions.
Fellowships cover the broad themes of Genetic and Molecular Basis of Disease; Pathogens, Infectious Disease and Immunity; Physiology, Pathophysiology and Experimental Medicine; Behaviour, Mental Health and Neurological Diseases; Epidemiology, Prevention and Public Health; Health Care Delivery and Improvement.
Application deadline: Monday 17 January 2022 (midday UK time).
Visit the Wellcome-MRC Institute of Metabolic Science website for further details or contact the Programme Administrator with any queries.
Key mutations in Alpha variant enable SARS-CoV-2 to overcome evolutionary weak points
One of the key mutations seen in the ‘Alpha variant’ of SARS-CoV-2 – the deletion of two amino acids, H69/V70 – enables the virus to overcome chinks in its armour as it evolves, say an international team of scientists.
SARS-CoV-2 is a coronavirus, so named because spike proteins on its surface give it the appearance of a crown (‘corona’). The spike proteins bind to ACE2, a protein receptor found on the surface of cells in our body. Both the spike protein and ACE2 are then cleaved, allowing genetic material from the virus to enter the host cell. The virus manipulates the host cell’s machinery to allow the virus to replicate and spread.
As SARS-CoV-2 divides and replicates, errors in its genetic makeup cause it to mutate. Some mutations make the virus more transmissible or more infectious, some help it evade the immune response, potentially making vaccines less effective, while others have little effect.
Towards the end of 2020, Cambridge scientists observed SARS-CoV-2 mutating in the case of an immunocompromised patient treated with convalescent plasma. In particular, they saw the emergence of a key mutation – the deletion of two amino acids, H69/V70, in the spike protein. This deletion was later found in B1.1.7, the variant that led to the UK being forced once again into strict lockdown in December (now referred to as the ‘Alpha variant’).
Now, in research published in the journal Cell Reports, researchers show that the deletion H69/V70 is present in more than 600,000 SARS-CoV-2 genome sequences worldwide, and has seen global expansion, particularly across much of Europe, Africa and Asia.
The research was led by scientists at the University of Cambridge, MRC-University of Glasgow Centre for Virus Research, The Pirbright Institute, MRC Laboratory of Molecular Biology, and Vir Biotechnology.
Professor Ravi Gupta from the Cambridge Institute of Therapeutic Immunology and Infectious Disease at the University of Cambridge, the study’s senior author, said: “Although we first saw this mutation in an immunocompromised patient and then in the Kent – now ‘Alpha’ – variant, when we looked at samples from around the world, we saw that this mutation has occurred and spread multiple times independently.”
Working under secure conditions, Professor Gupta and colleagues used a ‘pseudotype virus’ – a harmless virus that displays SARS-CoV-2 spike proteins with the H69/V70 deletion – to understand how the spike protein interacts with host cells and what makes this mutation so important.
When they tested this virus against blood sera taken from fifteen individuals who had recovered from infection, they found that the deletion did not allow the virus to ‘escape’ neutralising antibodies made after being vaccinated or after previous infection. Instead, the team found that the deletion makes the virus twice as infective – that is, at breaking into the host’s cells – as a virus that dominated global infections during the latter half of 2020. This was because virus particles carrying the deletion had a greater number of mature spike proteins on their surface. This allows the virus to then replicate efficiently even when it has other mutations that might otherwise hinder the virus.
“When viruses replicate, any mutations they acquire can act as a double-edged sword: a mutation that enables the virus to evade the immune system might, for example, affect how well it is able to replicate,” said Professor Gupta.
“What we saw with the H69/V70 deletion was that in some cases, the deletion helped the virus compensate for the negative effects that came with other mutations which allowed the virus to escape the immune response. In other words, the deletion allowed these variants to have their cake and eat it – they were both better at escaping immunity and more infectious.”
Dr Dalan Bailey from The Pirbright Institute, who co-led the research, added: “In evolutionary terms, when a virus develops a weakness, it can lead to its demise, but the H69/V70 deletion means that the virus is able to mutate further than it otherwise would. This is likely to explain why these deletions are now so widespread.”
Bo Meng from the Department of Medicine at the University of Cambridge, first author on the paper, said: “Understanding the significance of key mutations is important because it enables us to predict how a new variant might behave in humans when it is first identified. This means we can implement public health and containment strategies early on.”
The research was supported by Wellcome, the Medical Research Council, the Bill & Melinda Gates Foundation and the National Institute for Health Research (NIHR) Cambridge Biomedical Research Centre.
- The paper Recurrent emergence of SARS-CoV-2 spike deletion H69/V70 and its role in the variant of concern lineage B.1.1.7 is available online in the open-access journal Cell Reports.
Upgrading PPE for staff working on COVID-19 wards cut hospital-acquired infections dramatically
When Addenbrooke’s Hospital in Cambridge upgraded its face masks for staff working on COVID-19 wards to filtering face piece 3 (FFP3) respirators, it saw a dramatic fall – up to 100% – in hospital-acquired SARS-CoV-2 infections among these staff.
The findings are reported by a team at the University of Cambridge and Cambridge University Hospitals (CUH) NHS Foundation Trust. The research has not yet been peer-reviewed, but is being released early because of the urgent need to share information relating to the pandemic.
Until recently, advice from Public Health England recommended that healthcare workers caring for patients with COVID-19 should use fluid resistant surgical masks type IIR (FRSMs) as respiratory protective equipment; if aerosol-generating procedures were being carried out (for example inserting a breathing tube into the patient’s windpipe), then the guidance recommended the use of an FFP3 respirator. PHE has recently updated its guidance to oblige NHS organisations to assess the risk that COVID-19 poses to staff and provide FFP3 respirators where appropriate.
Since the start of the pandemic, CUH has been screening its healthcare workers regularly for SARS-CoV-2, even where they show no symptoms. They found that healthcare workers caring for patients with COVID-19 were at a greater risk of infection than staff on non-COVID-19 wards, even when using the recommended respiratory protective equipment. As a result, its infection control committee implemented a change in respiratory protective equipment for staff on COVID-19 wards, from FRSMs to FFP3 respirators.
Prior to the change in respiratory protective equipment, cases were higher on COVID-19 wards compared with non-COVID-19 wards in seven out of the eight weeks analysed by the team. Following the change in protective equipment, the incidence of infection on the two types of ward was similar.
The results suggest that prior to the change, almost all cases among healthcare workers on non-COVID-19 wards were caused by community-acquired infection, whereas cases among healthcare workers on COVID-19 wards were caused by both community-acquired infection and direct, ward-based infection from patients with COVID-19 – but that these direct infections were effectively mitigated by the use of FFP3 respirators.
To calculate the risk of infection for healthcare workers working on COVID-19 and non-COVID-19 wards, the researchers developed a simple mathematical model.
Dr Mark Ferris from the University of Cambridge’s Occupational Health Service, one of the study’s authors, said: “Healthcare workers – particularly those working on COVID-19 wards – are much more likely to be exposed to coronavirus, so it’s important we understand the best ways of keeping them safe.
“Based on data collected during the second wave of the SARS-CoV-2 pandemic in the UK, we developed a mathematical model to look at the risks faced by those staff dealing with COVID-19 patients on a day to day basis. This showed us the huge effect that using better PPE could have in reducing the risk to healthcare workers.”
According to their model, the risk of direct infection from working on a non-COVID-19 ward was low throughout the study period, and consistently lower than the risk of community-based exposure.
By contrast, the risk of direct infection from working on a COVID-19 ward before the change in respiratory protective equipment was considerably higher than the risk of community-based exposure: staff on COVID-19 wards were at 47 times greater risk of acquiring infection while on the ward than staff working on a non-COVID-19 ward.
Crucially, however, the model showed that the introduction of FFP3 respirators provided up to 100% protection against direct, ward-based COVID-19 infection.
Dr Chris Illingworth from the MRC Biostatistics Unit at the University of Cambridge, said: “Before the face masks were upgraded, the majority of infections among healthcare workers on the COVID-19 wards were likely due to direct exposure to patients with COVID-19.
“Once FFP3 respirators were introduced, the number of cases attributed to exposure on COVID-19 wards dropped dramatically – in fact, our model suggests that FFP3 respirators may have cut ward-based infection to zero.”
Dr Nicholas Matheson from the Department of Medicine at the University of Cambridge, said: “Although more research will be needed to confirm our findings, we recommend that, in accordance with the precautionary principle, guidelines for respiratory protective equipment are further revised until more definitive information is available.”
Dr Michael Weekes from the Department of Medicine at the University of Cambridge, added: “Our data suggest there’s an urgent need to look at the PPE offered to healthcare workers on the frontline. Upgrading the equipment so that FFP3 masks are offered to all healthcare workers caring for patients with COVID-19 could reduce the number of infections, keep more hospital staff safe and remove some of the burden on already stretched healthcare services caused by absence of key staff due to illness. Vaccination is clearly also an absolute priority for anyone who hasn’t yet taken up their offer.”
The research was funded by Wellcome, the Addenbrooke’s Charitable Trust, UK Research and Innovation, and the NIHR Cambridge Biomedical Research Centre.
- For a copy of the paper see: FFP3 respirators protect healthcare workers against infection with SARS-CoV-2.
Cambridge researchers win government funding for their artificial intelligence (AI) technologies
Technologies developed by Cambridge researchers that use artificial intelligence to speed up diagnosis and improve patient care have been successful in the latest round of the £140million Artificial Intelligence in Health and Care Award.
In total four AI projects, which Cambridge researchers either led or collaborated in, received funding, which was announced by Secretary of State for Health, Matt Hancock, on 16 June.
It means that the researchers will be able to take the technology one step closer to being used in the NHS to benefit patients.
AI-systems for improving blood transfusion outcomes
Professor Emanuele Di Angelantonio from the NIHR Blood and Transplant Research Unit in Donor Health and Genomics, Dr William Astle NHSBT Senior Lecturer in Statistical Science in the MRC Biostatistics Unit and their collaborators at UCLH, Oxford University and international blood services, have been awarded more than £1million to improve, develop and implement AI-systems for genetic blood group typing, the automated stocking of blood according to type and the precision matching of patients to blood units.
Professor di Angelantonio said: “There are over thirty known blood group systems and each system can create different blood types.
“For patients receiving regular blood transfusions, it’s vital that the blood they receive is compatible with their own. If the blood is not matched, it can cause complications which can get worse over time – but at the moment it costs the NHS a lot of time and money to run the tests that are needed to measure a complete set of blood groups.
“It is now very cheap to measure blood groups genetically – we hope to blood type 100,000 blood donors and 500 sickle cell disease patients genetically in 2021. This will allow us to use AI to match sickle cell disease patients – who stand to benefit hugely from more precise blood matching – to donors.”
Dr Astle added: “This NIHR AI Award funding will help us to extend and develop the AI methods required for genetic blood matching, which should reduce the avoidable harm caused by transfusion reactions in the NHS.
“This has the potential to transform the quality of clinical care for patients dependent on transfusion, who can become untransfusable if they regularly receive mismatched blood.”
AI-enabled spine fracture pathway
In this multi-centre study, five hospitals including Cambridge University Hospitals are using an AI solution to detect osteoporotic fractures and identify new patients for treatment.
Dr Ken Poole, who is leading the study in Cambridge, said: “Osteoporosis is a common bone disease. Breaking a bone in the spine is a clear sign of it, but many patients don’t even realise they have a spine fracture at the time. They mistake the symptoms for ordinary back pain, and ignoring that cue can then lead to a cascade of more spine fractures or even a hip fracture, with devastating consequences.
“Each year over two million people undergo scans that include the spine, for various reasons such as lung or bowel problems. Remarkably, up to one in 20 of people having these scans could have spine fracture, although very few fractures are recognised or acted upon.
“This project will use an innovative AI software that automatically looks at existing CT scans to find these fractures and brings them directly to the specialist team’s attention, to see if the patient needs bone-strengthening lifestyle advice and medicines.
“We believe that this ‘AI-enabled spine fracture pathway’ will improve patient health and reduce costs to hospitals – and ensure tens of thousands of adults with undetected spine fractures are identified and protected against having future potentially life-changing fractures.”
This project is being run with Zebra-Med, an AI and machine learning company headquartered in Israel.
AI to differentiate tumour and healthy tissue on cancer scans
Consultant oncologist Dr Raj Jena has received an AI Award for 12 months to accelerate the process of registering AI technology that can spot the difference between tumours and healthy tissue on cancer scans as a medical device.
Once registered, it can then begin to be rolled out across key NIHR BRCs.
The NIHR Cambridge and Birmingham BRCs are using open-source AI tools from Microsoft Project InnerEye to differentiate tumour from healthy tissue on cancer scans. This is called ‘segmenting’ and takes place prior to radiotherapy treatment.
Dr Jena said: “This saves clinicians’ time, and reduces the time between the scan and commencing radiotherapy treatment.”
Monitoring slow-growing brain tumours
Certain types of brain tumour are deemed low-risk, as they grow so slowly. This project, led by Hon. Consultant Neurosurgeon Stephen Price, aims to develop AI to measure the volume of tumours from scans, and learn which are at risk of growth, to ensure those patients are monitored more frequently, and others can be reassured that their tumour is lower risk.
Professor Miles Parkes, Director of the NIHR Cambridge BRC, said: “This is fantastic news and congratulations to everyone involved.
“The Award will help increase the impact of the AI-driven technologies that Ken, Emanuele, Will, Raj and Stephen are developing.
“Their innovations will not only offer faster and more personalised diagnosis, they will also provide the evidence we need to demonstrate the effectiveness and safety of AI-driven technologies in health and social care.
“The technologies our researchers are developing today have the potential to transform clinical care for thousands of patients across the country.”
Patient and Public Involvement and Engagement (PPI/E) Strategy Lead Dr Amanda Stranks said: “For these technologies to be successful in the clinic, it is essential that patients are at the heart of their design and usage.
“It’s also great to see the NIHR asking for clear evidence of strong patient and public involvement strategies in the projects they are funding.
“For example, the AI osteoporosis study under Ken Poole in Cambridge will have patients represented on the study steering committee, project management team and locally, to ensure the project remains patient-centred throughout its life cycle.
“The AI system for improving blood transfusion outcomes also has actively involved patients, including setting up a patient panel to advise on the project.”
- All the AI projects that receive awards will be independently evaluated for their effectiveness, safety and value in the NHS settings in which they are deployed. This will add to the evidence base and inform the onward adoption and scaling of the technology.
Updated risk model helps doctors predict and prevent cardiovascular disease
Research developing the European Society of Cardiology (ESC) cardiovascular disease (CVD) risk prediction calculator to aid efforts to reduce the burden of CVD in Europe has been published today by European Heart Journal.
The research – carried out by the SCORE2 Working Group and the ESC Cardiovascular Risk Collaboration – analysed data from nearly 700,000 mainly middle-aged participants in 45 large-scale studies to develop risk prediction models (SCORE2) tailored for use in European countries.
The participants did not have previous history of CVD at the outset and 30,000 had a CVD event (heart attack or stroke) during the first 10 years of follow up.
These risk models were then statistically adapted or ‘recalibrated’ to more accurately estimate CVD risk for contemporary populations in four European risk regions, using data on population-specific CVD incidence rates and risk factor values from 10.8 million individuals.
SCORE2 will replace the original SCORE (Systematic COronary Risk Evaluation) model, and is adopted by the upcoming European Guidelines on CVD Prevention in Clinical Practice.

Professor Di Angelantonio (pictured), who with Dr Lisa Pennells and Dr Stephen Kaptoge led the research from the University of Cambridge, said: “The original research focused solely on predicting and preventing mortality, using data from the 1980s.
“But now more people survive heart attacks and strokes than die from them, especially younger people, so we wanted to show the absolute risk scores of people having non-fatal as well as fatal CVD within 10 years.
“This new highly collaborative effort was developed using data from dozens of countries, including exceptionally powerful, extensive and complementary datasets of contemporary relevance to European populations.
“As this risk prediction tool is superior to its predecessors, it should have substantial real-world impact by improving the primary prevention of cardiovascular disease across Europe through helping doctors to identify high-risk patients who may benefit from lifestyle change or preventative medication.”
- SCORE2 risk prediction algorithms: revised models to estimate 10-year risk of cardiovascular disease in Europe was published by the European Heart Journal on 14 June 2021.
Join us in supporting International Clinical Trials Day
Every year 20 May is celebrated by healthcare workers, researchers, patients and communities around the world to mark International Clinical Trials Day.
On this day in 1747, ship surgeon James Lind started what is believed to be the world’s first randomised clinical trial, when he asked 12 sailors who all had scurvy to ingest six different treatments including cider, vinegar, sea water and an orange and lemon. Within days the man who had received the citrus fruit had recovered so much that he was appointed nurse to the others on the trial.
Make future research breakthroughs possible
To coincide with International Clinical Trials Day, the NIHR is running its Be Part of Research campaign.
This celebrates the thousands of people who volunteered to be part of research including taking part in the fight back against COVID-19. At the same time, the campaign encourages more people to take part in research to ensure future medical breakthroughs happen.
Being part of research: what our patients and volunteers say
- Volunteers are still needed for studies into all conditions, including diabetes, cancer, mental health and dementia: find out what research is taking place near you.
- Do you use Twitter? Include the #BePartofResearch hashtag and help promote the value of clinical research. Don’t forget to follow us on Twitter for more patient quotes about taking part in research!
Save your energy! New tool shows algorithms’ environmental impact
Data science and artificial intelligence are transforming UK healthcare – but at an environmental cost.
The data centres housing the supercomputers that run the algorithms account for 100 megatonnes of CO2 emissions every year – roughly the same as US commercial aviation. It takes more and more energy to run increasingly complex algorithms – and even a best-case scenario predicts a three-fold increase in the sector’s energy needs by 2030.
Now Cambridge scientists supported by the NIHR Cambridge BRC have developed a freely available tool which allows anyone to estimate the carbon footprint of their computations.
Dr Michael Inouye from the University of Cambridge, who supervised the development of Green Algorithms, said: “We’ve been using computers, supercomputers and cloud computation for many years now, yet there hasn’t been an easy way to work out how much greenhouse gases our computations emit.
“High-performance and large-scale computing have led to many scientific breakthroughs; for example, in astrophysics we now know what black holes 55 million light-years away look like, and in genomics, we now know of thousands of genetic variants for common diseases. We didn’t know the environmental impact of using data science to uncover these discoveries, nor did we have the tools to estimate what the next-generation of breakthroughs would take in terms of carbon footprint.
“So our team set about developing a free and easy-to-use online tool, Green Algorithms, for users to estimate the carbon footprint of any computational task.”
Know your computation’s carbon footprint
Want to know what the weather will be like tomorrow in your home town? A supercomputer in Reading will do that for you – at an environmental cost.
Using Green Algorithms, Dr Inouye’s team calculated that the computations it runs for just one day’s forecasts are equivalent in terms of greenhouse gas (GHG) emissions to driving 1,708 km or taking three return flights between Paris and London. It would take a mature tree over 27 years to sequester this amount of carbon.
Dr Inouye said: “Green Algorithms takes into account what’s ‘under the hood’ of a computer, the length of time it’s used and the location of the resources it utilises to estimate the energy used and the kilograms of CO2 emitted.
“It then shows the equivalent footprint in car and plane journeys, and ‘tree months’, or the number of months a mature tree needs to absorb a given quantity of carbon.
“Green Algorithms also makes specific recommendations for reducing computing’s carbon footprint. For example do you really want to continue using data centres which are heavily reliant on coal for power, even if they have faster processors? What would be the carbon savings or costs if you moved them elsewhere?
“Considerations like these better capture the true costs of computation, taking it beyond the purely financial.”
The carbon footprint of an algorithm depends on two factors: energy needed to run it and the GHG emissions released per unit of energy needed. This depends on the computing resources needed (including how long it takes to run, the number of cores and memory used and how efficient the data centre is) and the data centre’s location and what powers it (e.g. nuclear, gas or coal). Switching from an average data centre to a more efficient one can reduce carbon footprint by a third.
Computations are rarely performed only once. Algorithms are run multiple times, sometimes hundreds, and many are for good reasons but frequently they are unnecessary. This also increases GHG emissions, sometimes substantially. Limiting the number of times an algorithm runs is perhaps the easiest way to reduce unnecessary carbon footprint.
Director of the NIHR Cambridge BRC Professor Miles Parkes said: “We are delighted to have supported such timely and vital research, which has created an open tool for quantifying the carbon footprint of virtually any computation.
“The NIHR is committed to combating climate change and helping the UK meet the goals set forth in the Climate Change Act 2008.
“NIHR both promotes green approaches to health research and actively designs new tools that expand opportunities for green research that can be translated into policy and action.
“This tool empowers researchers, patients and the public to understand and minimise the greenhouse gas emissions of both their work and leisure, whether using home laptops, a high-performance computing cluster or the cloud.”
Dr Inouye added: “We hope our study will help raise awareness of the environmental impacts of day-to-day computer use and the computations underlying data science as well as promote more sustainable practices within the data science community.
“We want to make green computing a cornerstone of carbon reduction within the NHS, ensuring that the artificial intelligence revolution supports both a healthier society and planet.”
- The research paper Green Algorithms: Quantifying the carbon footprint of computation by lead authors Loïc Lannelongue and Jason Grealey, and Michael Inouye, is available to view on the open access journal Advanced Science.
- Find out more about this research and the hidden costs of computations in Advanced Science’s feature article on Green Algorithms: Quantifying the carbon footprint of computation.
- The NIHR Carbon Reduction Guidelines have been published to help researchers explore how they can apply the principles of good carbon management and sensible study design to reduce carbon footprint.
- Three days of action to highlight urgency of climate redress took place from 20-22 April, culminating in Earth Day 2021 on 22 April.
Differing immune responses discovered in asymptomatic cases and those with severe COVID-19
A UK-wide study part-funded by the NIHR has identified differences in people’s immune responses to COVID-19, depending on whether they have no symptoms or more serious reactions to the virus.
In the study “Single-cell multi-omics analysis of the immune response in COVID-19”, published this month in Nature Medicine, researchers and their collaborators in the Human Cell Atlas initiative analysed blood from 130 people with COVID-19. These patients came from three different UK centres in Newcastle, Cambridge and London and ranged from asymptomatic to critically severe.
The researchers found raised levels of specific immune cells in asymptomatic people to help fight infection – but that patients with more serious symptoms had lost these protective cell types and instead gained inflammatory cells. In severe cases this led to lung inflammation, blood clotting difficulties and hospitalisation.
While it is not yet understood how the infection stimulates these immune responses, the study gives a molecular explanation for how COVID-19 could cause an increased risk of blood clotting and inflammation in the lungs, which can lead to the patient needing a ventilator.
This also uncovers potential new therapeutic targets to help protect patients against inflammation and severe disease.
Professor Menna Clatworthy, senior co-author of the study and Capacity Building Theme Lead, said: “This is one of the most detailed studies of immune responses in COVID-19 to date, and begins to help us understand why some people get really sick while others fight off the virus without even knowing they have it.
“This new knowledge will help identify specific targets for therapy for patients who get sick with COVID-19.”
In the future, research may identify those who are more likely to experience moderate to severe disease by looking at levels of these immune cells in their blood.
Addenbrooke’s specialist endocrinology services ranked best in UK
In their annual specialist hospital rankings, Newsweek has rated the specialist diabetes and endocrinology services at Addenbrooke’s Hospital as the best in the UK, and 20th internationally. Patients attending clinics through this service benefit not only from the expertise of leading clinicians, but also from the state-of-the-art research programme supported by clinical academics and research partners through the NIHR Cambridge Biomedical Research Centre (NIHR Cambridge BRC).
Dr Tony Coll, Service Lead at the Wolfson Diabetes and Endocrine Clinic (WDEC) at Addenbrooke’s said: “This recognition is a testament to many decades of focused effort to meaningfully link academic efforts with high quality patient care.”
WDEC is at the forefront in using new technologies such as insulin pumps and glucose sensors to improve the lives of people with diabetes. WDEC is contained within the Wellcome-MRC Institute of Metabolic Science (IMS), a purpose-built centre dedicated to research and clinical care in the areas of diabetes, endocrinology and related diseases. Close collaboration between researchers and clinicians through the NIHR Cambridge BRC, IMS and other research partners has enabled translation of advances in research of the genetic basis, diagnosis and treatment of disorders of insulin and thyroid hormone action into clinical practice.
For children up to 15 years, the Weston Children’s Diabetes and Endocrine Service provides excellent clinical care both during childhood and transition whilst benefitting from the most recent advances in translational research. Major advances pioneered in collaboration between research partners and the services include closed loop insulin delivery (the ‘artificial pancreas’) and strategies to detect and prevent early complications through the AdDIT trial.
The ‘artificial pancreas’ works by combining an insulin pump with constant glucose monitoring via a sensor fitted on the skin. The sensor sends information about the level of glucose in the blood to an app that directs the insulin pump to maintain the correct dosage of insulin. Together, these technologies significantly simplify life for people with type 1 diabetes, particularly during night and for very young patients.
Cambridge is also a lead in a major EU consortium (INNODIA) which supports research with people newly diagnosed with type 1 diabetes and their relatives, including access to clinical studies and trials designed to prevent further progression following diagnosis.
Professor Sir Stephen O’Rahilly MD FRS FMedSci, Co-Director of the Wellcome-MRC Institute of Metabolic Science and Scientific Director, NIHR Cambridge Biomedical Research Centre said of the ranking: “The Wellcome-MRC Institute of Metabolic Science was created with the vision of linking basic and applied research in endocrine and metabolic diseases with excellent clinical care. The Newsweek ranking provides evidence that the Institute is being recognised by colleagues around the world for the quality and inventiveness of its work at the interface between research and patient care.”
Prof Miles Parkes, Director of the NIHR Cambridge BRC, congratulated the team, saying: “This recognition clearly reflects the hard work of the endocrinology theme and partners, leading innovative discovery science and integrating it into world-leading clinical care. The vital importance of translational research and its clinical implementation is sometimes less heralded, but the diabetes and endocrine team have demonstrated how critical it is to improving patient outcomes and supporting the NHS. They are truly deserving of the recognition they have received for their work.”
POPStar study launches to investigate how pregnancy data can predict future health
A new study from the Departments of Obstetrics & Gynaecology and Paediatrics at the University of Cambridge is investigating how conditions in the womb can predict the future health of mothers and their children.
 The POPstar study will look at the anonymised data of over 4,000 mother-child pairs who participated in the NIHR-funded Pregnancy Outcome Prediction Study (POPS) and link it to data from the NHS, Department of Education and other agencies to see if growth patterns are associated with high risk of health or developmental problems.
The POPstar study will look at the anonymised data of over 4,000 mother-child pairs who participated in the NIHR-funded Pregnancy Outcome Prediction Study (POPS) and link it to data from the NHS, Department of Education and other agencies to see if growth patterns are associated with high risk of health or developmental problems.
POPS recruited pregnant women at the Rosie from 2008-12 and using interviews, blood samples and extra scans, collected very detailed information on pregnancy outcomes, and growth and development in the womb.
Dr Catherine Aiken from the research team said: “This information is a unique resource and has already been used to draw important conclusions about the immediate health of mothers and babies.
“We now want to see if we can use this data to help predict the likelihood of health problems for both mum and child, including long-term maternal health and developmental delay and neurodisability for the child.
“This is a really exciting opportunity to find new ways of identifying problems early, for example children at risk of developmental delay.
“If we know who is high-risk, then we have measures that can help, such as early learning support.”
Contribution
The POPS children are now aged between six and ten years, and have already contributed a huge amount to clinical care teams’ understanding of birth complications. Professor Gordon Smith, chief investigator for both POPS and POPstar and co-lead for our Women’s health and paediatrics theme, said: “This is a really good example of making the most of the information that is routinely collected to go further in improving the future health of mothers and their children.”
- POPStar is funded jointly by the NIHR Cambridge BRC and the children’s charity Action Medical Research.
- To find out more visit the study website or contact the research team at popstarstudy@medschl.cam.ac.uk.
Prestigious fellowship election for NIHR Cambridge BRC researchers
The NIHR Cambridge BRC is delighted that three of our researchers have been elected as Fellows of the Academy of Medical Sciences.
Theme leads Professor Menna Clatworthy and Professor Ludovic Vallier, together with Professor Ziad Mallat, who is one of our researchers in the Cardiovascular and respiratory disease theme, are among 50 world-leading UK researchers who have been elected to the prestigious Fellowship.
To be elected to the Academy, Fellows must have made exceptional contributions to advancing biomedical science.
In the current coronavirus global health crisis, the value of medical science has never been more apparent and like many Academy Fellows, Professors Vallier, Mallat and Clatworthy have redirected their research efforts to tackle the effects of the pandemic.
Professor Vallier’s team has developed a technology to grow a type of cell in the bile duct known as cholangiocytes in vitro (in test-tubes), so that they can study the effects of coronavirus on the liver. Professor Vallier said: “These liver cells express high levels of the SARS-CoV2 receptors and can be infected by the virus.
“We are using this model to study how the virus can enter cells and also to identify drugs which could limit this process.”
Professor Mallat’s team is studying how SARS-CoV2 infection can lead to heart attacks, and examining whether and how medications that alter the way the immune system works can modify cardiovascular outcomes.
Professor Mallat said: “This work is in close collaboration with investigators of the TACTIC trial and with many investigators in the Department of Medicine, and is also supported through BHF-CRE funding.”
Professor Clatworthy’s team is helping to study blood samples taken as part of the TACTIC-R trial, applying cutting-edge technologies to white blood cells (the body’s defence cells) to understand why some people experience an over-active immune response to the virus, and to look at the effect of the trial drugs on this response.
- Professors Clatworthy, Vallier and Mallat join Dr Helen Firth, Professor Tamsin Ford and Dr Nitzan Rosenfeld from the University of Cambridge who were also elected Fellows. Read more about the announcement on the University of Cambridge website.
Fast-track HRA review of COVID-19 studies
The Health Research Authority (HRA) is working with the rest of the research system to provide a coordinated process so that COVID-19 research can progress quickly, using a fast-track review process with bespoke advice and support for researchers.
The average review timeline is 5 days, with many completed within 24 to 72 hours.
HRA have updated the information on their website about the fast-track review process, guidance for researchers, sites and sponsors, guidance about using confidential patient data without consent and information about how it is handling other types of research.
This review takes place in parallel with the Chief Medical Officer’s prioritisation process for COVID studies.
To ensure that information about COVID-19 related research is made public as quickly as possible, summary information about each COVID-19 research project is available on the HRA website.
New National guidance for prioritising funding and support for COVID-19 research across the UK
Published by NIHR 26 March 2020:
Working with partners across the health and care system, NIHR is leading, enabling and delivering world-class COVID-19 research, a key element of the Government’s overall response to the pandemic. Given the extraordinary pressures currently being faced by the health and care system, we must also ensure that we are making best use of the limited resources and capacity available to support research.
We will do this by establishing and implementing a single, national process that will allow the Chief Medical Officer (CMO) / Deputy Chief Medical Officer (DCMO) for England to draw on expert advice to prioritise the COVID-19 studies which hold the most potential for tackling the challenges we face.
This process will cover all funded studies, irrespective of whether they are funded by the public sector, industry or charities and also, in partnership with UKRI, studies that require funding. It aims to prevent duplication of effort and to ensure that the capacity of the health and care system to support research is not exceeded.
Details of the process and the new single point of entry for prioritising COVID-19 studies can be found here.
With regard to HRA approvals, researchers should make an application through the national prioritisation process first and will be signposted for expedited regulatory approvals so that approval review can progress in parallel to the system of assessment leading to a view from CMO/DCMO on prioritisation.
All NHS Trusts, health and care providers and universities will need to prioritise support for studies which have been nationally prioritised. A live list of these studies is being collated. Organisations may support COVID-19 research activity only when this does not impact on the system’s ability to recruit participants and/or provide the resources (including staff, samples and data) needed to support nationally prioritised research. Organisations will be expected to pause any local studies that impede their ability to contribute to national research efforts.
- Government support for research related to COVID-19: Find out how to get your study nationally supported or funded as high priority COVID-19 Urgent Public Health Research.
- COVID-19 and Clinical Research Oversight Group CUH: This has been established under the governance of the NIHR Cambridge BRC and will review nationally prioritised studies to consider which can be supported locally with the available resources.
- NIHR response to COVID-19 pandemic: All NIHR updates on one page.
- Covid-19 response from the NIHR Cambridge BRC: Information for researchers, academics and clinicians on clinical research taking place on the Cambridge Biomedical Campus during the COVID-19 outbreak.
COVID-19 research studies at CUH
In response to the COVID-19 pandemic Cambridge University Hospitals has put in place measures to help researchers and research infrastructure deliver COVID-19 studies, whilst also supporting the care of patients with COVID-19 by redeployment of resources where necessary.
Chief and Principal Investigators of studies have been reviewing whether part or all of their studies need to be put on hold. Many existing studies are now suspended, and the NIHR Clinical Research Network is pausing any studies that are not nationally prioritised COVID-19 studies.
The NIHR has emphasised the need to prioritise COVID-related work, and are putting in place mechanisms for fast-tracking nationally prioritised studies through HRA and MHRA. A COVID-19 and Clinical Research Oversight Group has been established under the governance of the NIHR Cambridge BRC and will review nationally prioritised studies to consider which can be supported locally with the available resources.
The group will also consider proposals for studies to be sponsored by Cambridge University Hospitals and / or the University of Cambridge, but these are likely to need to have national reach or build on unique local capability to meet the threshold for fast -tracking through HRA / MHRA approval processes.
Professor Ian Wilkinson, Director of the Cambridge Clinical Trials Unit (CCTU), is also establishing a committee to review proposals for clinical trials related to COVID-19.
If you have questions, research proposals or clinical trials that you wish to be considered please contact Covid19research@addenbrookes.nhs.uk in the first instance.
Medovate working with CUH team to bring life-saving upper GI therapy device to market
Medical device company Medovate has secured the exclusive rights to bring to market a pioneering endoscopic surgical device.
The new device, ENDOVAC, has the potential to dramatically improve survival of patients with life-threatening infection following a leak from their the upper gastrointestinal (GI) tract whilst significantly enhancing current treatment methods.
Developed by a team led by Mr Andrew Hindmarsh (pictured left in photo), Consultant Oesophagogastric Surgeon at Cambridge University Hospitals, ENDOVAC is also backed by a £1.2m grant from the National Institute for Health Research, which has a number of regional specialist partners including the Hospital, the Cambridge Clinical Trials Unit, Health Enterprise East and Suffolk-based JEB Technologies Ltd. Medovate’s role is to attain regulatory approval and commercialise this technology, with a view to beginning clinical evaluation as early as 2021 and market launch thereafter.
Each year, around 2,800 people in the UK get a hole in their upper GI tract. These holes may occur on their own; arise from problems such as stomach ulcers; or be caused through surgery or other medical interventions. The presence of a hole allows leakage of gastrointestinal contents into the body which quickly leads to infection around vital organs such as the heart and lungs, a serious medical emergency that is fatal if not treated successfully.
In the past, the standard treatment for these holes has been surgery, but this was often unsuccessful. More recently surgeons have developed an alternative treatment strategy for this problem called Endoluminal Vacuum Therapy (EVT). However, this treatment still needs improvement as it requires multiple technically difficult procedures under general anaesthesia in an operating theatre to be successful.
ENDOVAC is a ground-breaking progression of EVT. This novel technology allows easier delivery of treatment without the need for general anaesthesia, meaning the procedure does not need to be performed in an operating theatre. ENDOVAC makes EVT safer, quicker, easier and cheaper, and importantly is far less traumatic for patients. It will also enable patients to be mobile during treatment, unlike standard EVT, where patients are often confined to their hospital beds.
Robert Donald, New Business Manager at Medovate (pictured right in photo), commented: “ENDOVAC offers a deceptively simple solution to a complex problem that has sadly claimed many lives over the years. The team at Cambridge University Hospitals have come up with a straightforward yet effective device [and] we are excited to be working with Mr Hindmarsh and his colleagues to bring such a ground-breaking product to market.”
Update on clinical research during the COVID-19 outbreak
UPDATE 7 APRIL 2020:
Approval process for COVID-19 related research
Locally, trials and studies need first to be reviewed by the Cambridge BRC/Covid-19 oversight committee before being submitted through the national NIHR prioritisation mechanism.
All COVID-19-related research studies are being prioritised at a national level through the NIHR. Studies seeking approval should first apply through the NIHR gateway, with nationally prioritised research being signposted for an expedited regulatory approval with the HRA/MHRA.
Email Covid19research@addenbrookes.nhs.uk for more information about undertaking COVID-19-based research studies at CUH.
Continue reading previous update (dated 19 March 2020):
As part of our response to COVID-19, some of our research activity will need to change.
We are reviewing all of our clinical research with Cambridge University Hospitals (CUH) and the University of Cambridge. Each study is being assessed on a case-by-case basis to minimise risks to participants either from continued participation in or disruption to a trial that forms part of their clinical care.
Some studies will need to pause or wind down to release staff for clinical roles and sample processing infrastructure to support the NHS.
Principal Investigators:
Chief and Principal investigators should review their studies and assess the risk to participants posed by COVID-19. Following risk assessment, please confirm your proposed mitigations or actions with Professor John Bradley, Director of Research, as soon as possible.
Research Participants:
Research participants will be contacted by their study team with updates about any changes to the study they are enrolled in. Please contact your study team if you have any further questions about your study or your participation during these events. Participants who believe they have COVID-19 symptoms should follow Department of Health and Social Care advice and contact their study team.
Patient and Public Involvement (PPI):
CUH is committed to supporting the research effort against COVID-19, and patients and the public will have a particularly valuable role as we embark on this. The PPI team are working remotely, but are still available to speak to researchers who need assistance with PPI for their grant applications or documentation reviewed by the CUH PPI panel. Our panel has over 70 people who are willing to review research-related documents and this service is still available, with our panel members very committed to continuing their support for researchers during this period.
Non-essential visits to the campus are not permitted at this time. As such, we have cancelled all in-person meetings and training that were planned through to the summer. This will continue to be reviewed as the situation changes. All filming and work experience in our research buildings have been suspended/ cancelled due to the current restrictions in place.
The PPI and communications team are also investigating options to run their training sessions and other PPI activities online.
If you need any assistance contact the PPI team: cuh.ppi@nhs.net
It’s your data – so have your say in how it should be used
How do you think health data should be shared and used – and who should share it?
Now’s your chance to tell Cambridge researchers what you think about accessing, sharing and using YOUR health data – in an online survey from the CLIMB research project.
The survey should only take you about 20 minutes and will ask you questions about your views on sharing your health data for both clinical and research purposes. The information you provide will be anonymous.
You can find out more about CLIMB and what the survey is aiming to achieve on their website.
Who can take part?
- Anyone who lives in the UK – this is a national survey
- Anyone who is over 16 – children under 16 can also take part, as long as they have their parent’s/guardian’s permission
I use local services in Cambridge – what options do I choose for questions about where I heard about the survey?
- NIHR Cambridge BRC is not an option, simply choose where applicable “Hospital” and then “Addenbrooke’s”
Please feel free to forward to family and friends, far and wide! You can do it for or on behalf of children and remember, it only takes about 20 minutes.
Begin the survey.
New NIHR Cambridge BRC director appointed
The NIHR Cambridge Biomedical Research Centre (BRC) has announced Dr Miles Parkes will be the new director of the centre, based at Cambridge University Hospitals (CUH).
Dr Miles Parkes is currently a consultant gastroenterologist and researcher at CUH.
His research focuses on understanding the causes of Crohn’s disease and ulcerative colitis, and the factors that affect the course and outcomes of treatment for these conditions – by focusing on their genetics and the gut microbiota. In addition he researches new ways of managing and treating Crohn’s disease and ulcerative colitis.
Miles already leads the UK IBD genetics consortium and is also the clinical and academic lead for the recently established Health Data Research Hub for IBD, known as Gut Reaction.
Miles will take over the role from Professor John Bradley, who announced in late 2019 he would be stepping down from his director role at the NIHR Cambridge BRC. John will still play an integral part in the development of research on the Cambridge Biomedical Campus as he continues to be joint director of the NIHR BioResource and Research and Development Director at CUH.
Research in Cambridge
The NIHR Cambridge BRC is a partnership between Cambridge University Hospitals and the University of Cambridge which is located at the Cambridge Biomedical Campus and funded by the NIHR. Biomedical Research Centres aim to bring academics and the hospital together to speed up research in order to create new treatments and medicines for the benefit of patients and the NHS.
The NIHR Cambridge BRC is one of the largest BRCs in England and has significant expertise in the major health challenges we face today such as antimicrobial resistance, cancer, dementia, diabetes, mental health and obesity.
Since its creation in 2007, the centre has already delivered medical breakthroughs including a new screening device to detect Barrett’s oesophagus and the use of genomic testing for rapid diagnosis of critically ill babies.
Miles will begin his new role on 01 April 2020. He will work with clinicians and industry partners on the campus to deliver ground-breaking research in Cambridge. Miles said: “I’m delighted to have been appointed as the new director of the NIHR Cambridge BRC. It’s a big remit, and John Bradley has given me a tough act to follow. However, the opportunities for translational research in Cambridge are enormous.
“By working with colleagues across the whole biomedical campus, I hope we can all push to accelerate the clinical translation of the many medical and scientific advances being made each week in Cambridge. We will strive to continue the success of the NIHR Cambridge BRC and bring forward improved patient care.”
Professor Patrick Maxwell, Regius Professor of Physic and Head of the School of Clinical Medicine said: “I am absolutely delighted with the appointment of Dr Parkes to lead the NIHR Cambridge Biomedical Research Centre.
“Miles is an excellent gastroenterologist and has a fantastic track-record in developing important insights into inflammatory bowel disease. John Bradley, the founding Director of the BRC, is a really hard act to follow but I have complete confidence that Miles will be an outstanding leader of our translational research partnership.”
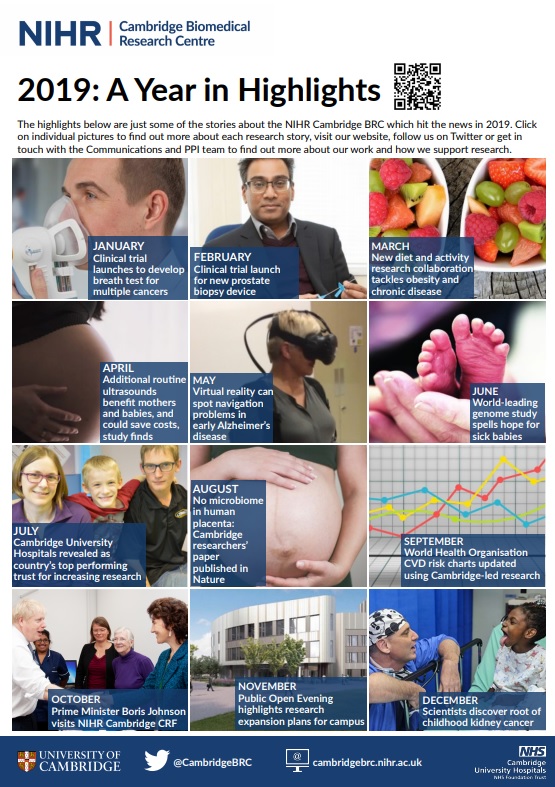
NIHR Cambridge BRC research highlights over 2019
From breath tests for cancer to finding the root of childhood kidney cancer, what are the research stories that NIHR Cambridge BRC supported or funded which hit the news over 2019? Click on the picture below to bring up our highlights, then select a picture to find out more about each news story.
We’ve picked a story for every month of 2019 – but we’ve also funded and supported much more. Go to our theme or publications pages to find out more.
Winning research poster at our Open Evening unveiled – as voted for by you!
Is DNA your destiny?
Not necessarily, according to Cambridge postdoctoral researcher Dr Kousik Kundu – whose poster was voted the public’s favourite at the NIHR Cambridge BRC Open Evening which took place last November.
The poster was one of 13 on display highlighting individual research projects which the NIHR Cambridge BRC and local colleagues have supported and funded, and which were chosen for their readability and accessibility to a lay audience. It was then up to members of the public to select their favourite!
Dr Kundu’s winning poster, which was a collaboration with Professor Nicole Soranzo and fellow researchers at the Wellcome Sanger Institute, summed up his team’s research in the genetic factors underlying individuals’ disposition to life-changing diseases.
Dr Kundu said: “While we share 99.9% of our genomes with other people, it is that 0.1% that can affect our susceptibility to any disease and our response to medicines.
“By understanding these genomic differences we can work out the best possible way to treat a patient for a range of diseases – from diabetes and heart disease to cancer.
“But our research showed that environmental factors, such as our lifestyle and diets, also play an important role on how we respond to a drug – and that it could be possible to develop better therapeutic approaches to personalised healthcare.”
In designing the poster Dr Kundu said: “I learnt a lot about how to make a very complex scientific work simple and attractive, while providing a very important message which can be easily understood by a lay audience.
“I think because of its simplicity, many people found my poster interesting and stopped to ask many questions.”
Communications and PPI Strategy Lead Amanda Stranks said: “The standard of entries for our Open Evening was incredibly high, but Kousik’s colourful use of graphics and non-technical language ensured that his poster neatly got across why the research was necessary and its impact.”
Dr Kundu’s current research focuses on the genetic factors of several immune-mediated diseases, such as Crohn’s disease, rheumatoid arthritis and multiple sclerosis. He is also working to generate whole genome sequence data from UK Biobank samples and to analyse data from the NIHR-funded INTERVAL study, which showed that blood donors could safely give blood more frequently than is allowed at present without having a major impact on their health.
He said: “We are possibly not far away from when doctors will prescribe the right combination of medicines at the right time that is most suitable for an individual.”
- Dr Kundu’s current research focuses on the genetic factors of several immune-mediated diseases, such as Crohn’s disease, rheumatoid arthritis and multiple sclerosis
- Click to view “Genomics and Personalised Medicine” poster.