‘Biological fingerprint’ in blood could help identify COVID patients with no symptoms
Cambridge researchers are able to identify people who have had COVID-19 even if they displayed no symptoms. They have developed a way to find markers in the blood several months after infection, even if the individual had only mild or showed no symptoms at all.
Most people who have COVID-19 may recover in a few weeks but there are some who will develop severe symptoms that can last for several months.
Current practice requires people to take a PCR test at the time of infection or an antibody test, looking at the immune cells, to reveal if someone may have previously had the virus but were asymptomatic. Now Cambridge researchers have discovered a biomarker – a biological fingerprint – in the blood of patients who previously had COVID-19.
This has led the team to receive £370,000 from the National Institute for Health Research (NIHR) to develop a COVID-19 diagnostic test that will complement existing antibody tests, as well as develop a test that could diagnose and monitor long Covid.
The research builds on a pilot project supported by the Addenbrooke’s Charitable Trust which has been recruiting patients from the Long COVID Clinic established in May 2020 at Addenbrooke’s Hospital.
Finding the biomarker
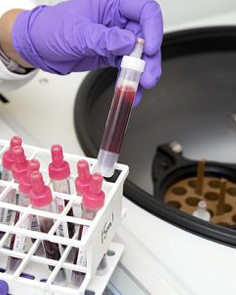
During the pilot, the team recruited 85 patients to the Cambridge-led NIHR COVID BioResource, which collects blood samples from patients when they are first diagnosed and then at follow-up intervals over several months.
In their initial findings, they identified a molecule known as a cytokine produced by T cells in response to infection. As with antibodies, this biomarker persists in the blood for a long time after infection.
Dr Mark Wills from the Department of Medicine at the University of Cambridge, who co-leads the team, said: “We need a reliable and objective way of saying whether someone has had COVID-19. Antibodies are one sign we look for, but not everyone makes a very strong response and this can wane over time and become undetectable.
“We’ve identified a cytokine that is also produced in response to infection by T cells and is likely to be detectable for several months – and potentially years – following infection. We believe this will help us develop a much more reliable diagnostic for those individuals who did not get a diagnosis at the time of infection.”
By following patients for up to 18 months post-infection, the team hopes to address several questions, including whether immunity wanes over time. This will be an important part of helping understand whether people who have been vaccinated will need to receive boosters to keep them protected.
As part of their pilot study, the team also identified a particular biomarker found in patients with long COVID. Their work suggests these patients produce a second type of cytokine, which persists in patients with long COVID compared to those that recover quickly and might be one of the drivers behind the many symptoms that patients experience. This might therefore prove to be useful for diagnosing long COVID.
Dr Nyarie Sithole, also from the Department of Medicine at the University of Cambridge, who co-leads the team and helps to manage long COVID patients, said: “Because we currently have no reliable way of diagnosing long COVID, the uncertainty can cause added stress to people who are experiencing potential symptoms. If we can say to them ‘yes, you have a biomarker and so you have long COVID’, we believe this will help allay some of their fears and anxieties.
“There is anecdotal evidence that patients see an improvement in symptoms of long COVID once they have been vaccinated – something that we have seen in a small number of patients in our clinic. Our study will allow us to see how this biomarker changes over a longer period of time in response to vaccination.”
At the moment, the team is using the tests for research purposes, but by increasing the size of their study cohort and carrying out further work, they hope to adapt and optimise the tests that can be scaled up and speeded up, able to be used by clinical diagnostic labs.
As well as developing a reliable test, the researchers hope their work will help provide an in-depth understanding of how the immune system responds to coronavirus infection – and why it triggers long COVID in some people.
Dr Sithole added: “One of the theories of what’s driving long COVID is that it’s a hyperactive immune response – in other words, the immune system switches on at the initial infection and for some reason never switches off or never goes back to the baseline. As we’ll be following our patients for many months post-infection, we hope to better understand whether this is indeed the case.”
In addition, having a reliable biomarker could help in the development of new treatments against COVID. Clinical trials require an objective measure of whether a drug is effective. Changes in – or the disappearance of – long-COVID-related cytokine biomarkers with corresponding symptom improvement in response to drug treatment would suggest that a treatment intervention is working.
Understanding COVID-19
An extensive programme of 15 new research studies, backed by government funding through the NIHR, will allow researchers across the UK to draw together their expertise from analysing long COVID among those suffering long-term effects and the health and care professionals supporting them. These groundbreaking studies aim to help those people affected return to their normal lives.
Health and Social Care Secretary, Sajid Javid, said: “Long COVID can have serious and debilitating long term effects for thousands of people across the UK, which can make daily life extremely challenging.
“This new research is absolutely essential to improve diagnosis and treatments and will be life-changing for those who are battling long-term symptoms of the virus.
“It will build on our existing support with over 80 long COVID assessment services open across England as part of a £100 million expansion of care for those suffering from the condition and over £50 million invested in research to better understand the lasting effects of this condition.”