Identifying those at risk from liver failure
Researchers from Cambridge wanted to understand PBC, how it affects patients and whether they would be able to predict those who would be at risk of liver failure.
Working alongside the NIHR BioResource – a resource of thousands of volunteers who wish to take part in research, researchers looked at a group of 2,000 patients with PBC who use ursodeoxycholic acid (UDCA) to help with their condition.
From studying this large group of people and samples given, they were able to identify high-risk patients who could go on to develop liver failure and would need a liver transplant within the next 15 years.
After further investigations, researchers created an accurate scoring tool to identify patients at risk. Clinicians can now recognise patients who need to be closely monitored, or who may need extra therapies and identify those who are appearing as low risk.
The Risk Score Calculator has been adopted as part of national guidance from the Advisory Committee for the Safety of Blood Tissues and Organs and many hospitals are now using the tool.
Screening babies earlier to prevent complications later
Using ultrasound scans, a study was conducted to look at growth restriction in babies before they were born and whether the scans could be an indicator of any problems before birth.
The women who participated were offered extra scans in the later stages of their pregnancy so researchers could investigate the growth of their baby in the womb. Then after they had given birth, the babies were measured, and tissue samples from the placenta and umbilical cord were collected.
After scanning more than 4,500 women, researchers were able to demonstrate that extra scans from 24 weeks could be a predictor of adverse pregnancy outcome. However, they are working now on whether biomarkers might improve such prediction when combined with the scan results.
It is hoped that women could potentially be identified as a ‘high risk’ using these new screening tests before they experience complications. Doctors would then be able to act to prevent complications to themselves or the unborn baby.
Using whole genome sequencing to fight common bugs
Cambridge researchers wanted to investigate how these ‘resistant’ bacteria could be identified faster, so that outbreaks can be reduced and treatments can be given sooner to patients who may be diagnosed with an infection.
Researchers looked at using whole genome sequencing or WGS (a complete set of all the genes of the bacteria including those causing resistance) and examined whether this technique would be an effective mechanism to detect these infectious threats as well as understand their biology and how they are spreading.
Researchers found they were able to identify the bacteria and their resistance patterns (e.g. which antibiotics work and which do not) directly from clinical samples taken from patients, using information gleaned from WGS. They noticed that using WGS gave more accurate information about the microbes and that it provided much better and much more detailed information than normal laboratory methods.
Researchers are continuing to look at ways of improving how these technologies can prevent the spread of infections and improve treatment selection.
How DNA technologies are helping pneumonia patients fight back
The antimicrobial resistance team have been working with researchers from Public Health England and clinicians in the Intensive Care Unit at Cambridge University Hospitals to better understand the different types of pneumonia patients may have and to try and identify if they have an infection faster.
To do this, they are using revolutionary DNA-analysis and sequencing technologies that can help them identify exactly which microbes (if any) are contributing to a patient’s pneumonia. Using these technologies, researchers are now able to screen for around 100 kinds of microbes within hours of a sample being taken from the patient and identify which is the best antibiotic to use. Also some patients look like they are infected but are not and these can be quickly picked up. They can also identify how the patient is responding to the infection and help guide better treatment.
Quick identification of the right microbe will enable researchers to select and develop the right antibiotics to fight infection and prevent the disease from developing in vulnerable patients.
Diagnosing autism in adulthood
Many patients are overlooked or misdiagnosed, seeing a variety of clinical specialists before they receive a diagnosis.
The Cambridge team were keen to improve the referral and so developed a new screening tool called the Autism Spectrum Quotient (AQ) for front-line clinicians and social care professionals.
The AQ is a questionnaire designed by the researchers to evaluate how many autistic traits a person has. If a patient’s scores are high, the tool alerts clinical staff to make a referral for a full assessment. It was first developed in 2001 and was one of the first metrics of the autism spectrum. The full questionnaire has 50 items but the Cambridge team produced a brief version of just 10 items, known as the AQ-10.
This new diagnosis tool provides a quick but reliable indicator that someone may potentially have undiagnosed autism, therefore ensuring their referral for a diagnosis is both more accurate and quantitative, not just based on opinion. Ensuring that the right patients are referred to the specialist clinics means a better use of clinic time and a quicker journey from the referrer to the final assessment.
Once diagnosed, the patient can then be helped to access the support and therapies they require. The AQ has been used widely in research studies, and in 2013 NICE guidelines it was recommended for use with adults with suspected autism or Asperger Syndrome. The tool is now used widely both nationally and internationally.
New app to help people with OCD symptoms
One common behaviour of people with OCD symptoms is repeated hand washing, to prevent a feeling of contamination. Excessive washing can be harmful, however, causing problems such as skin damage as well as reducing people’s mental health and wellbeing. Furthermore, severe contamination fears may prevent people from leaving their own homes.
Compulsive behaviours are related to ‘cognitive rigidity’ – finding it difficult to adapt to new situations or rules and consider alternative behaviours or responses. Current treatments are not effective for all sufferers, with up to 40% of patients not experiencing significant benefit from the most common options.
Cambridge researchers have developed a new treatment to help with excessive hand washing through an app. A study to test the new app used otherwise healthy patients who had expressed strong fears of contamination on the Padua Inventory Contamination Fear Subscale, which is a questionnaire commonly used by researchers to measure concerns associated with contamination.
Participants who used the app to watch videos of washing their hands or touching contaminated surfaces had reduced feelings of contamination and improved cognitive flexibility.
Further research is needed and researchers hope the technology will help people manage their symptoms and experience better quality of life and wellbeing.
Expecting a boy or girl could influence pregnancy risks
Researchers studied more than 4,000 first-time mothers by analysing blood samples and the placenta. They found that the placental genes controlled a small molecule called spermine – a metabolite which is a substance involved in the metabolism. This molecule is important in all cells and essential for the growth of some bacteria.
They observed female placentas had a high level of the enzyme that makes spermine, and women who were pregnant with girls had a higher level of spermine in their blood compared to women who were pregnant with boys. So these findings might explain why women expecting a girl are more at risk of complications such as pre-eclampsia and women expecting a boy are more at risk of the baby not growing at a normal rate inside the womb.
This research could help doctors predict women who are at higher risk of pregnancy complications.
Genetic study identifies genetic mutations in PAH patients
Researchers in Cambridge carried out the largest ever genetic study of the disease by analysing the genomes – the DNA – of more than 1,000 people with PAH.
They discovered that mutations in several genes were responsible for causing the illness, including four genes that were not previously known to be connected to the disease. The mutations cause some proteins to stop working well, contributing to the arterial stiffness.
Understanding the causes of the disease will help researchers to better target new treatments to help people with PAH.
The defibrillator that gets under your skin
It usually results when the heart beats with rapid erratic electrical impulses (known as ventricular fibrillation) and arises in a person with underlying heart disease. Those at risk of sudden cardiac arrest can be given an Implantable Cardiac Defibrillator (ICD), which sends shocks to the heart to restore normal cardiac rhythm. The ICD is placed under the skin and leads are passed through a vein into the heart.
ICDs can cause problems when the device for example deteriorates or breaks down and then there is a risk for the patient. Researchers in Cambridge developed a subcutaneous ICD (S-ICD) which can be placed under the skin, removing the need for surgery or having the device wired up to the heart.
The device successfully completed clinical trials which resulted in European approval (2009) and FDA approval in the United States (2012) and is routine treatment in most UK Specialist Centres.
Over 50,000 people have now benefited from the S-ICD worldwide. In October 2013 the S-ICD was awarded the Prix Galien (‘regarded as equivalent Nobel Prize in biopharmaceutical research’) in New York as the ‘Best Medical Technology’.
Most guidelines now regard the S-ICD as an option of choice for most patients for both the primary and secondary prevention of sudden cardiac death.
More information about this research can be heard by Nick Morrell, in the video above.
Screening for dementia in the community
CANTAB Mobile,which runs on an iPad, includes a learning and memory test as part of a cognitive trial. Researchers are using these tests in GP settings to detect early stages of Alzheimer’s disease. From the data collected, researchers will determine if this kind of testing in a primary care setting can detect patients earlier, before the disease progresses, allowing doctors to act earlier and put a treatment plan in place. Early therapeutic interventions are beneficial as they allow patients to stay in their homes for longer and delay institutionalised care. They also enhance quality of life for people with dementia and their carers.
Could Virtual Reality help detect the earliest stages of Alzheimer’s disease?
The three-year project – led by Dr Dennis Chan at the University with joint funding from the Alzheimer’s Society, Merck and NIHR Cambridge BRC – will scale up earlier research in which Dr Chan’s team showed that a VR test of spatial navigation was more effective at identifying patients with mild cognitive impairment (MCI) due to Alzheimer’s disease (AD) than gold standard tests of memory and thinking currently used in clinic and research studies.
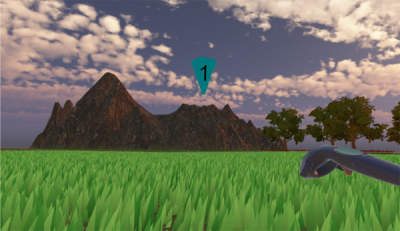
Participants (like the one photographed, above) were asked to navigate within virtual environments, displayed in state-of-the-art immersive VR headsets. This involved walking to, then remembering, the location of cones displayed within the environment. (See above image for an example: clicking on the image will open a short demonstration video.)
Now Dr Chan’s team would like to see if this test can detect AD in even earlier stages, before the onset of cognitive impairment.
In this latest study, researchers will ask 300 volunteers aged between 40 and 60, without any memory impairment, to take part in the VR study.
The volunteers have already enrolled into the PREVENT dementia programme, and have differing risks of developing AD depending on whether they have a gene that puts them at risk of AD or if they have a family history of AD.
Dr Chan’s prediction is that those at higher risk of future AD will perform less well on the VR navigation task.
Coco Newton, a PhD student on Dr Chan’s team, said: “Alzheimer’s disease is notoriously hard to detect in the early stages, when it is known as ‘preclinical’ AD. But if we can show that a VR-based navigation test is more accurate than traditional memory tests in diagnosing the preclinical disease, then that opens up lots of exciting opportunities.
“Not least it will allow people to determine whether treatments are more effective if they are started earlier and if this can delay the onset of dementia.
“By diagnosing patients much sooner we will also be able to offer them the opportunity to take part in clinical trials of future treatments.”
Testing navigation – virtually
The headset used in the study will be familiar to computer gamers.
Ms Newton explained: “You just place the headset on your face like a pair of goggles, and you are immediately placed in your ‘virtual’ environment. The headset displays images that are then used to test navigational skills as you walk around. Ultimately we want to find out if those who do worse in the tests will develop AD in later life.”
Find out more
Detecting AD in its earliest stages |
|---|
| It’s a tiny area of the brain, but scientists believe that the entorhinal cortex within the temporal lobe (which is involved in navigation) is the first to be affected by AD. But by the time the patient has developed symptoms such as memory problems, years or decades after the disease process has started, a substantial proportion of brain cells will already have degenerated.
What Dr Chan and his team want to find out is whether changes to the entorhinal cortex can be detected in people at risk of developing dementia using VR and other cutting-edge technology including bespoke apps and augmented reality. People at risk of AD and healthy volunteers will be selected to take part in all the tests, including the VR navigation test. Some participants will also undergo state-of-the-art brain scanning with ultra high resolution 7T MRI and tau-PET scanning which can detect the molecules associated with AD pathology. |
NIHR Applied Research Collaborations (ARC)
NIHR ARC East of England focuses its research efforts on the needs of people with complex problems, often vulnerable when multiple agencies are involved in their care: young people, frail older people, those with dementia, learning disabilities, acquired brain injuries or mental ill health.
The ARC collaboration encompasses some thirty-six organisations, with research hubs in the Universities of Cambridge, Hertfordshire and East Anglia working closely with individuals and organisations involved in the whole care pathway.
Clinical Trials Pharmacy
The team also have growing experience with Advanced Therapy IMPs and work closely with Cambridge Cellular Therapy Laboratory to provide pharmaceutical governance for studies involving cellular treatments.
Pharmacy clinical trial support is an integral part of the research process and has a vital role to play in safeguarding participants, healthcare professionals and the Trust by ensuring IMPs and other study medications are appropriate for use and are procured, handled, stored and used safely and correctly in line with regulatory requirements. A dedicated Clinical Trials Dispensary is on site and pharmacy aseptic dispensing facilities are also available.
For Trust-sponsored Clinical Trials of IMPs (CTIMPs), pharmacy are involved from the outset of a project and work closely with Cambridge Clinical Trials Unit to advise on costings for grant applications, protocol design and review of the overall trial application in relation to medication, including manufacturing and participating site aspects. Pharmacy will also advise on non-CTIMP research as required.
Cancer Research UK Cambridge Centre
Our mission is to end death and disease caused by cancer, through research, treatment and education. As one of just two Cancer Research UK Major Centres, we serve as a national and international resource for patients with cancer and their families; researchers and health care providers; and cancer professionals in training.
The Cancer Research UK Cambridge Centre facilitates new collaborations and drives the translation of new scientific discoveries into clinical applications to improve patient care. By working together across a range of different disciplines, our members are breaking down the barriers between the laboratory and the clinic, enabling patients to benefit from the latest innovations in cancer science.
NIHR Research Design Service
RDS advisers offer a unique breadth of experience in helping both novice and more experienced researchers to develop competitive research applications. Advice is confidential and free of charge.
If you are developing a research proposal to attract NIHR/other National competitive funding, please complete the RDS client enquiry form on the RDS East of England website. An adviser will contact you to set up an initial meeting to talk through your research ideas and to get an understanding of why the research is important. As the grant application evolves, advisers will provide on-going advice on the study design and methods, and will help to ensure that the research team has the required expertise. They will signpost you to the relevant departments and organisations that you will need to liaise with when developing a competitive application. The RDS holds regular bid development workshops and also offers ‘pre-submission’ panels.
To request support complete this form or click on our leaflet
EMBL-European Bioinformatics Institute (EMBL-EBI)
At EMBL-EBI, we perform basic research in bioinformatics, make the world’s public biological data freely available to the scientific community via a range of services and tools, and provide professional training in bioinformatics.
We are part of the European Molecular Biology Laboratory (EMBL), an international, innovative and interdisciplinary research organisation funded by 23 member states and two associate member states.
Headway Cambridgeshire
Headway Cambridgeshire provides specialist services to people with an acquired brain injury and other neurological conditions and their families and carers.
Brain injury can affect anybody, at any time. Headway Cambridgeshire supports people through these life-changing events, building bespoke services to meet their needs and aspirations and helping people to live as independently as possible and achieve their full potential.
With two hubs in Peterborough and Fulbourn, they offer a programme of activities and specialist services aimed at recovery and social rehabilitation. Working across the county of Cambridgeshire, the charity provides information, hospital liaison, occupational therapy, community enablement and the opportunity to participate in social events.
Cambridgeshire Lupus Group
Cambridgeshire Lupus Group gives a local point of contact to help, support and give general advice to people with Systemic, Cutaneous and Discoid Lupus and associated conditions.
The group supports members through information and education about Lupus and the latest developments in its treatment. By arranging events, local support meetings, publishing a local newsletter and working with health professionals to increase the awareness of lupus.
Cambridgeshire Lupus Group supports the young person’s lupus group at Addenbrooke’s Hospital.
Facebook: Cambridgeshire Lupus Group
About Lupus
Systemic Lupus Erythematosus (SLE or lupus) is a presently incurable, but in most cases manageable, illness of the immune system, a condition in which the body’s defence mechanism begins to attack itself through an excess of antibodies in the blood stream causing inflammation and damage in the joints, muscles and other organs.
The majority of lupus patients are young women aged 16-55 but men and even young children can be affected.
Lupus may be triggered by various means and can present in a bewildering number of ways, even to the extent of mimicking other illnesses such as Rheumatoid Arthritis or Multiple Sclerosis. The cause of lupus is not known, although research has provided evidence implicating heredity, hormones, environmental factors and infections including viruses.
Inflammation, infection and immunotherapeutic theme
Lipodystrophy UK
Lipodystrophy UK is a patient support group for patients who have the rare disease lipodystrophy, which covers a group of conditions characterised by the lack of subcutaneous fat (normal fat storage under the skin). Lipodystrophy can be generalised (total fat loss) or partial (partial fat loss) and familial (inherited) or acquired (not inherited).
The inability to store fat under the skin causes fat to be stored in places such as the muscles and liver which leads to severe metabolic complications including insulin resistance, diabetes, dyslipidaemia, heart disease, kidney disease, fatty liver disease and many others. Currently, there is no cure for Lipodystrophy and only the secondary complications can be managed/treated. Lipodystrophy affects approximately 1 in 1 million people across the world.
Metabolism, endocrinology and bone theme
Breathe Easy Cambridge Support Group
Breathe Easy Cambridge Support Group is a local patient support group who meet in Cambridge on the 3rd Tuesday of every month at St Catherine’s Road, Cambridge, CB4 3 XJ between 14:00 and 16:00. The group are part of the British Lung Foundation and more information can be found on their website.
Breathe Easy Cambridge Support Group supports patients, carers and family members living with a lung condition.