Artificial pancreas successfully trialled for use by type 2 diabetes patients
Cambridge scientists have successfully trialled an artificial pancreas for use by patients living with type 2 diabetes. The device – powered by an algorithm developed at the University of Cambridge – doubled the amount of time patients were in the target range for glucose and halved the time spent experiencing high glucose levels.
Around 415 million people worldwide are estimated to be living with type 2 diabetes, which costs around $760 billion in annual global health expenditure. According to Diabetes UK, in the UK alone, more than 4.9million people have diabetes, of whom 90% have type 2 diabetes, and this is estimated to cost the NHS £10bn per year.
Type 2 diabetes causes levels of glucose – blood sugar – to become too high. Ordinarily, blood sugar levels are controlled by the release of insulin, but in type 2 diabetes insulin production is disrupted. Over time, this can cause serious problems including eye, kidney and nerve damage and heart disease.
The disease is usually managed through a combination of lifestyle changes – improved diet and more exercise, for example – and medication, with the aim of keeping glucose levels low.
Researchers from the Wellcome-MRC Institute of Metabolic Science at the University of Cambridge and supported by the NIHR Cambridge BRC, have developed an artificial pancreas that can help maintain healthy glucose levels. The device combines an off-the-shelf glucose monitor and insulin pump with an app developed by the team, known as CamAPS HX. This app is run by an algorithm that predicts how much insulin is required to maintain glucose levels in the target range.
The researchers have previously shown that an artificial pancreas run by a similar algorithm is effective for patients living with type 1 diabetes, from adults through to very young children. They have also successfully trialled the device in patients with type 2 diabetes who require kidney dialysis.
Today, in Nature Medicine, the team report the first trial of the device in a wider population living with type 2 diabetes (not requiring kidney dialysis). Unlike the artificial pancreas used for type 1 diabetes, this new version is a fully closed loop system – whereas patients with type 1 diabetes need to tell their artificial pancreas that they are about to eat to allow adjustment of insulin, for example, with this version they can leave the device to function entirely automatically.
The researchers recruited 26 patients from the Wolfson Diabetes and Endocrine Clinic at Addenbrooke’s Hospital, part of Cambridge University Hospitals NHS Foundation Trust, and a local group of GP surgeries. Patients were randomly allocated to one of two groups – the first group would trial the artificial pancreas for eight weeks and then switch to the standard therapy of multiple daily insulin injections; the second group would take this control therapy first and then switch to the artificial pancreas after eight weeks.
The team used several measures to assess how effectively the artificial pancreas worked. The first was the proportion of time that patients spent with their glucose levels within a target range of between 3.9 and 10.0mmol/L. On average, patients using the artificial pancreas spent two-thirds (66%) of their time within the target range – double that while on the control (32%).
A second measure was the proportion of time spent with glucose levels above 10.0mmol/L. Over time, high glucose levels raise the risk of potentially serious complications. Patients taking the control therapy spent two-thirds (67%) of their time with high glucose levels – this was halved to 33% when using the artificial pancreas.
Average glucose levels fell – from 12.6mmol/L when taking the control therapy to 9.2mmol/L while using the artificial pancreas.
The app also reduced levels of a molecule known as glycated haemoglobin, or HbA1c. Glycated haemoglobin develops when haemoglobin, a protein within red blood cells that carries oxygen throughout the body, joins with glucose in the blood, becoming ‘glycated’. By measuring HbA1c, clinicians are able to get an overall picture of what a person’s average blood sugar levels have been over a period of weeks or months. For people with diabetes, the higher the HbA1c, the greater the risk of developing diabetes-related complications. After the control therapy, average HbA1c levels were 8.7%, while after using the artificial pancreas they were 7.3%.
No patients experienced dangerously-low blood sugar levels (hypoglycaemia) during the study. One patient was admitted to hospital while using the artificial pancreas, due to an abscess at the site of the pump cannula.

Dr Charlotte Boughton from the Wellcome-MRC Institute of Metabolic Science at the University of Cambridge, pictured right, who co-led the study, said: “Many people with type 2 diabetes struggle to manage their blood sugar levels using the currently available treatments, such as insulin injections. The artificial pancreas can provide a safe and effective approach to help them, and the technology is simple to use and can be implemented safely at home.”
Dr Aideen Daly, also from the Wellcome-MRC Institute of Metabolic Science, said: “One of the barriers to widespread use of insulin therapy has been concern over the risk of severe ‘hypos’ – dangerously low blood sugar levels. But we found that no patients on our trial experienced these and patients spent very little time with blood sugar levels lower than the target levels.”
Feedback from participants suggested that participants were happy to have their glucose levels controlled automatically by the system, and nine out of ten (89%) reported spending less time managing their diabetes overall. Users highlighted the elimination of the need for injections or fingerprick testing, and increased confidence in managing blood glucose as key benefits. Downsides included increased anxiety about the risk of hypoglycaemia, which the researchers say may reflect increased awareness and monitoring of glucose levels, and practical annoyances with wearing of devices.
The team now plan to carry out a much larger multicentre study to build on their findings and have submitted the device for regulatory approval with a view to making it commercially available for outpatients with type 2 diabetes.
Paper Reference
Daly, AB, Boughton, CK, et al. Fully automated closed-loop insulin delivery in adults with type 2 diabetes: an open-label, single-centre randomised crossover trial. Nat Med; 11 Jan 2023; DOI: 10.1038/s41591-022-02144-z
Professor Krishna Chatterjee awarded a CBE
Congratulations to Professor Krishna Chatterjee, consultant endocrinologist at Cambridge University Hospitals and director of NIHR Cambridge Clinical Research Facility who has been awarded a CBE in the King’s New Year Honours for his ground-breaking work on endocrine disorders.
Professor Chatterjee is also a professor of endocrinology at the University of Cambridge and led the COVBOOST vaccine trial locally during the pandemic. His research group focuses on genetic and molecular endocrinology, exploring disorders including resistance to thyroid hormone (RTH) and PPARgamma gene defects associated with lipodystrophic insulin resistance. He was awarded a CBE for his services to people with endocrine disorders.
He said: “I am delighted that our work has been recognised in this way. This also represents the efforts of many clinical and scientist colleagues in the University, CUH and our NIHR Clinical Research Facility, with whom I have worked over many years.
“Together with the patients participating in our research, we strive to continue advancing knowledge and health outcomes in endocrine disorders.”
Blood thinning drug to treat recovery from severe Covid is not effective
A UK-wide trial, led by Addenbrooke’s Hospital and the University of Cambridge, has found that a drug used to reduce the risk of blood clots does not help patients recovering from moderate and severe Covid – despite this approach being offered to patients.
The HEAL-COVID trial (Helping to Alleviate the Longer-term consequences of Covid-19) is funded by the NIHR and the NIHR Cambridge Biomedical Research Centre. To date, more than a thousand NHS patients hospitalised with Covid have taken part in HEAL-COVID, a platform trial that is aiming to find treatments to reduce the number who die or are readmitted following their time in hospital.
In these first results from HEAL-COVID, it’s been shown that prescribing the oral anticoagulant Apixaban does not stop Covid patients from later dying or being readmitted to hospital over the following year (Apixaban 29.1%, versus standard care 30.8%).
As well as not being beneficial, anticoagulant therapy has known serious side effects, and these were experienced by participants in the trial with a small number of the 402 participants receiving Apixaban having major bleeding that required them to discontinue the treatment.
There was also no benefit from Apixaban in terms of the number of days alive and out of hospital at day 60 after randomisation (Apixaban 59 days, versus standard care 59 days).
Following these results, the trial will continue to test another drug called Atorvastatin, a widely used lipid lowering drug (‘a statin’) that acts on other mechanisms of disease that are thought to be important in Covid.

Chief Investigator for the trial Professor Charlotte Summers, is an intensive care specialist at Addenbrooke’s Hospital and the University of Cambridge, pictured right, said: “Having survived the ordeal of being hospitalised with Covid-19, far too many patients find themselves back in hospital, often developing longer-term complications as a result of the virus. There is an urgent need for us to find treatments that prevent this significant burden of illness and improve the lives of so many still being affected by Covid.”
“These first findings from HEAL-COVID show us that a blood thinning drug, commonly thought to be a useful intervention in the post-hospital phase is actually ineffective at stopping people dying or being readmitted to hospital. This finding is important because it will prevent unnecessary harm occurring to people for no benefit. It also means we must continue our search for therapies that improve longer term recovery for this devastating disease.”

Dr Mark Toshner, joint Chief Investigator for HEAL-COVID, pictured left, said: “Up until now it’s been assumed that Apixaban helps patients recover after severe Covid-19 and that thinning their blood to prevent clots is beneficial. This trial is the first robust evidence that longer anticoagulation after acute Covid-19 puts patients at risk for no clear benefit.
“Our hope is that these results will stop this drug being needlessly prescribed to patients with Covid-19 and we can change medical practise. Finding out that a treatment doesn’t work is really important. It’s not the solution many hoped it would be, with our results highlighting once again why testing treatments in randomised trials is important.”
“At present, the world’s research efforts have focussed on acute Covid-19. We now urgently need evidence about how to best treat patients beyond their initial infection.”
Professor Nick Lemoine, NIHR Clinical Research Network Medical Director, said: “Research into Covid-19 recovery remains vital as we move out of the pandemic. Results such as these from the HEAL-COVID study, help to strengthen our knowledge of how patients can be treated following their stay in hospital and how recovery rates can be improved upon.
“Findings from clinical trials, whether they identify new treatments or rule out methods of care, are vital and rigorous evidence when it comes to changing best medical practice.”
The trial is being led by Cambridge University Hospitals NHS Foundation Trust (CUH) and University of Cambridge, in collaboration with Liverpool Clinical Trials Centre (University of Liverpool) and Aparito Limited.
HEAL-COVID enrols patients when they are discharged from hospital, following their first admission for Covid-19. They are randomised to a treatment and their progress tracked.
Cambridge researchers listed among world’s most influential researchers
Congratulations to our NIHR Cambridge BRC theme leads who have been named in the Clarivate listings of the ‘world’s most influential researchers’.
The researchers were selected on their exceptional research influence and highly cited research papers that rank in the top 1% by citations on the global database, Web of Science, over the last decade.
The full list of Cambridge researchers can be found on the Clarivate website.
| Name | Title | Associated theme |
|---|---|---|
| Professor Ed Bullmore | Honorary Consultant Psychiatrist and Head of the Department of Psychiatry | Mental Health |
| Professor John Danesh | Professor of Epidemiology | Population and quantitative sciences |
| Professor Ravindra K. Gupta | Professor of Clinical Microbiology | Antimicrobial resistance |
| Professor David Rowitch | Developmental neuroscientist and Head of Department of Paediatrics | Women’s health and paediatrics |
High blood pressure is directly linked to severe COVID-19
A study led by Addenbrooke’s Hospital and the University of Cambridge has shown that people with high blood pressure are more likely to be admitted to hospital or die from COVID-19, regardless of other factors such as age, sex, ethnicity or BMI.
The research, published this week in the Journal PLOS ONE, is the first study to show the extent to which high blood pressure, known as hypertension, can be directly linked to patients developing severe COVID-19.
It also showed that the type of medication people were receiving to treat hypertension did not appear to modify this risk. In addition, those patients who had poorly controlled blood pressure i.e. above treatment targets, were at the highest risk of dying or being hospitalised.
The study findings may help explain why ethnic minority and low-income groups were disproportionately affected by COVID-19, as hypertension is more common in these individuals, and rates of blood pressure control poorer (see notes).
The research has important implications for public health priorities, given that hypertension is already the leading risk factor for death in the UK.
It also comes as rates of blood pressure control have worsened in the UK, due to the pandemic, with the number or people being screened and identified with the condition dropping as well (see notes).
Holly Pavey is lead author of the study and a British Heart Foundation (BHF) funded PhD student at the University of Cambridge. She said:
“Before this research, it wasn’t clear to what extent high blood pressure was putting patients at greater risk of hospitalisation or dying from COVID-19. Other factors such as age, socio-economic status, sex, ethnicity and BMI were all in the frame too as increasing the risk of severe COVID-19.
“By using data from many thousands of UK volunteers, we found that in individuals who tested positive for COVID-19, those with high blood pressure had a 22% higher risk of being hospitalised of dying from the virus, compared to those without high blood pressure. This risk was almost doubled for those with poorly controlled blood pressure.”
The research was supported by the NIHR Cambridge Biomedical Research Centre and use data from the UK Biobank, a research database, containing in-depth genetic and health information from half a million UK volunteers. The study included over 16,000 of these individuals who had tested positive for COVID-19 and who had linked GP records, death records and COVID-19 lab results.
Researchers analysed data up until early 2021, which helped to reduce any bias from new variants of the virus, which were much more transmissible, as well as reducing any bias from the effects of widespread vaccinations.
However, the UK Biobank volunteer population is generally healthier than the general UK population and has relatively few participants from ethnic minority groups, so generalisations to the wider UK population need to be undertaken with caution.
Even though the death and hospitalisation rate due to COVID-19 has been hugely reduced over the last year due to virus mutations, the NHS vaccination program and availability of effective treatments, this research highlights the importance of having well-controlled blood pressure, in case of new, more severe strains of COVID-19 or other viruses in the future.
Ian Wilkinson, a cardiology consultant at Cambridge University Hospitals NHS Foundation Trust (CUH) and Professor of Therapeutics at the University of Cambridge, is the study’s senior author. He said: “Hypertension remains the leading risk factor for death in the UK and worldwide, despite effective treatments, and disproportionately affects low income groups and individuals from ethnic minority backgrounds.
“Our findings further emphasise the importance of adequate blood pressure control. Unfortunately, post-pandemic, the rates of blood pressure control have worsened, as have the number of people being screened and identified as having high blood pressure. This is now a major public health problem in the UK and needs to be addressed as part of the levelling-up agenda”.
A national trial is currently underway to improve treatments for hypertension, specifically for people from black, Asian and minority ethnic communities. At the moment most treatments have been tested mainly on white people and it’s not known if these are as effective on other ethnic groups.
The AIM HY trial is led by Professor Ian Wilkinson and Phil Chowienczyk, Professor of Clinical Cardiovascular Pharmacology, Kings College London and Chief Investigator for the trial.
Professor Chowienczyk said: “These findings highlight the importance of good blood pressure control, especially in individuals disproportionately affected by high blood pressure and COVID-19, such as those in ethnic minority groups in the UK. The AIM HY_INFORM trial is a major study, funded by the BHF and Medical Research Council, that will determine which drugs are most effective at lowering blood pressure in ethnic minority groups in the UK. This should report at the end of 2023 and will be instrumental in shaping new guidelines for the treatment of hypertension in the UK.”
World-first trial to transfuse lab-grown red blood cells is underway in Cambridge
Red blood cells that have been grown in a laboratory have now been transfused into another person at the NIHR Cambridge Clinical Research Facility in a world first clinical trial.
The manufactured blood cells were grown from stem cells from donors. The red cells were then transfused into volunteers in the RESTORE randomised controlled clinical trial.
This is the first time in the world that red blood cells that have been grown in a laboratory have been given to another person as part of a trial into blood transfusion.
If proved safe and effective, manufactured blood cells could in time revolutionise treatments for people with blood disorders such as sickle cell and rare blood types. It can be difficult to find enough well-matched donated blood for some people with these disorders.
The RESTORE trial is a joint research initiative by NHS Blood and Transplant and the University of Bristol, working with the University of Cambridge, Guy’s and St Thomas’ NHS Foundation Trust, NIHR Cambridge Clinical Research Facility, and Cambridge University Hospitals NHS Foundation Trust. It is part-funded by a NIHRH grant and supported by NIHR Cambridge BRC.
The trial is studying the lifespan of the lab grown cells compared with infusions of standard red blood cells from the same donor. The lab-grown blood cells are all fresh, so the trial team expect them to perform better than a similar transfusion of standard donated red cells, which contains cells of varying ages.
Additionally, if manufactured cells last longer in the body, patients who regularly need blood may not need transfusions as often. That would reduce iron overload from frequent blood transfusions, which can lead to serious complications.
The trial is the first step towards making lab grown red blood cells available as a future clinical product. For the foreseeable future, manufactured cells could only be used for a very small number of patients with very complex transfusions needs. NHSBT continues to rely on the generosity of donors.
Two people have so far been transfused with the lab grown red cells in Cambridge. They were closely monitored and no untoward side effects were reported. They are well and healthy. The identities of participants infused so far are not currently being released, to help keep the trial ‘blinded’.
The amount of lab grown cells being infused varies but is around 5-10mls – about one to two teaspoons.
Donors were recruited from NHSBT’s blood donor base. They donated blood to the trial and stem cells were separated out from their blood. These stem cells were then grown to produce red blood cells in a laboratory at NHS Blood and Transplant’s Advanced Therapies Unit in Bristol. The recipients of the blood were recruited from healthy members of the NIHR BioResource.
A minimum of 10 participants will receive two mini transfusions at least four months apart, one of standard donated red cells and one of lab grown red cells, to find out if the young red blood cells made in the laboratory last longer than cells made in the body.
Further trials are needed before clinical use, but this research marks a significant step in using lab grown red blood cells to improve treatment for patients with rare blood types or people with complex transfusion needs.

Chief Investigator Professor Cedric Ghevaert, Professor in Transfusion Medicine and Consultant Haematologist the University of Cambridge and NHS Blood and Transplant, pictured right, said: “We hope our lab grown red blood cells will last longer than those that come from blood donors. If our trial, the first such in the world, is successful, it will mean that patients who currently require regular long-term blood transfusions will need fewer transfusions in future, helping transform their care.”
Co-Chief Investigator Dr Rebecca Cardigan, Head of Component Development NHS Blood and Transplant and Affiliated Lecturer at the University of Cambridge said: “It’s really fantastic that we are now able to grow enough red cells to medical grade to allow this trial to commence, we are really looking forward to seeing the results and whether they perform better than standard red cells.”
Cambridge BRC receives £86.2 million to translate research discoveries into new treatments for patients
The National Institute for Health and Care Research (NIHR) has awarded £86.2 million to NIHR Cambridge Biomedical Research Centre (BRC) investigators to continue their ground-breaking research, translating new scientific insights into state-of-the-art diagnostics and treatments to transform healthcare. The Cambridge funding is one of 20 such awards granted to leading NHS and University partnerships across the country.
NIHR Biomedical Research Centres bring together the expertise of academic research and healthcare professionals. The Cambridge centre is a partnership between Cambridge University Hospitals and the University of Cambridge, taking advantage of the respective strengths and expertise of both organisations to create the ideal environment for cutting-edge ‘translational’ research – where scientific discoveries from the laboratory are turned into experimental and clinical trials to show their benefit, and ultimately improve care.
This is the fourth round of Biomedical Research Centre funding and builds on the outstanding research contributions of the past 15 years. Since its creation in 2007, the NIHR Cambridge BRC is recognised globally as a leading centre for translational research and is now one of the largest BRCs in England. It hosts world-leading experts in numerous specialties and state-of-the art infrastructure to conduct translational research.
The centre has already delivered medical breakthroughs including a new screening device to detect Barrett’s oesophagus, a condition that can lead to oesophageal cancer, the artificial pancreas to help patients with Type 1 Diabetes better manage their condition and the use of whole genome sequencing for rapid diagnosis of critically ill babies and children. NIHR Cambridge BRC also played a key role in responding to the COVID-19 pandemic through the ability to rapidly mobilise expertise and equipment to diagnose COVID-19, making major contributions to our understanding of the evolution of SARS-CoV2 variants, how the virus spreads through hospitals and other settings and leading on crucial trials to investigate new treatments to prevent long-term complications in survivors of COVID.
Realising the potential of cutting-edge research

The Cambridge Biomedical Campus hosts many world-leading experts and research institutes, together with the renowned hospitals of Addenbrooke’s, the Rosie and the Royal Papworth. The NIHR Cambridge BRC brings together these researchers and institutions to focus on translating their discoveries into new diagnostics and treatments.
Over the next five years, Cambridge will continue research in areas such as cancer, dementia and cardiovascular and respiratory diseases, as well as focusing on developing areas of technology that will likely revolutionise NHS care in the coming years, such as artificial intelligence (AI), genomic medicine and new state of the art imaging techniques.
The funding also provides opportunities for a diverse range of professionals to undertake research, building a new generation of leading researchers – including expanding research expertise in allied health professionals, such as physiotherapists, radiologists and dietitians.

Professor Miles Parkes, Director of NIHR Cambridge BRC said: “The NIHR Cambridge BRC has been instrumental in delivering many exciting advances over the past 15 years, building on Cambridge’s historic strengths in discovery science and translating these into improved diagnostics and treatments.
“Together with our clinical partners, our diverse pool of world-leading scientists and first-class research facilities make the Cambridge Biomedical Campus an ideal place to conduct ground-breaking translational research.
“This new funding reflects confidence in the continued innovation, strength and dedication of our research teams. Over the next five years we will be particularly focusing on early detection and the changes that lead to disease, so we can aim to prevent and reverse serious health conditions before irreversible damage occurs. We will leverage our strengths in genomic medicine and data science to support this research and work with patients and investigators regionally and nationally, to deliver world-class translational research and improve health outcomes.’’
Professor Lucy Chappell, Chief Executive of the NIHR, said: “Research by NIHR Biomedical Research Centres has led to a number of ground-breaking new treatments, such as new gene therapies for haemophilia and motor neurone disease, the world-first treatment for Creutzfeldt–Jakob disease, a nose-drop vaccine for whooping cough, and the first UK-wide study into the long-term impact of COVID-19.
“This latest round of funding recognises the strength of expertise underpinning health and care research across the country and gives our nation’s best researchers more opportunities to develop innovative new treatments for patients.”
NIHR Cambridge BRC themes
Watch this short video to find out what our research themes are and the work we will be doing over the next five years.
Read the full press release from the Department of Health.
Dementia signs detected as early as nine years ahead of diagnosis
Cambridge scientists have shown that it is possible to spot signs of brain impairment in patients as early as nine years before they receive a diagnosis for one of a number of dementia-related diseases.
In research published in Alzheimer’s & Dementia: The Journal of the Alzheimer’s Association, the team analysed data from the UK Biobank and found impairment in several areas, such as problem solving and number recall, across a range of conditions.
The findings raise the possibility that in the future, at-risk patients could be screened to help select those who would benefit from interventions to reduce their risk of developing one of the conditions, or to help identify patients suitable for recruitment to clinical trials for new treatments.
There are currently very few effective treatments for dementia or other neurodegenerative diseases such as Parkinson’s disease. In part, this is because these conditions are often only diagnosed once symptoms appear, whereas the underlying neurodegeneration may have begun years – even decades – earlier. This means that by the time patients take part in clinical trials, it may already be too late in the disease process to alter its course.
Until now, it has been unclear whether it might be possible to detect changes in brain function before the onset of symptoms. To help answer this question, researchers at the University of Cambridge and Cambridge University Hospitals NHS Foundation Trust turned to UK Biobank, a biomedical database and research resource containing anonymised genetic, lifestyle and health information from half a million UK participants aged 40-69.
As well as collecting information on participants’ health and disease diagnoses, UK Biobank collected data from a battery of tests including problem solving, memory, reaction times and grip strength, as well as data on weight loss and gain and on the number of falls. This allowed them to look back to see whether any signs were present at baseline – that is, when measurements were first collected from participants (between five and nine years prior to diagnosis).
People who went on to develop Alzheimer’s disease scored more poorly compared to healthy individuals when it came to problem solving tasks, reaction times, remembering lists of numbers, prospective memory (our ability to remember to do something later on) and pair matching. This was also the case for people who developed a rarer form of dementia known as frontotemporal dementia.
People who went on to develop Alzheimer’s were more likely than healthy adults to have had a fall in the previous 12 months. Those patients who went on to develop a rare neurological condition known as progressive supranuclear palsy (PSP), which affects balance, were more than twice as likely as healthy individuals to have had a fall.
For every condition studied – including Parkinson’s disease and dementia with Lewy bodies – patients reported poorer overall health at baseline.
First author Nol Swaddiwudhipong, a junior doctor at the University of Cambridge, said: “When we looked back at patients’ histories, it became clear that they were showing some cognitive impairment several years before their symptoms became obvious enough to prompt a diagnosis. The impairments were often subtle, but across a number of aspects of cognition.
“This is a step towards us being able to screen people who are at greatest risk – for example, people over 50 or those who have high blood pressure or do not do enough exercise – and intervene at an earlier stage to help them reduce their risk.”
Senior author Dr Tim Rittman from the Department of Clinical Neurosciences at the University of Cambridge added: “People should not be unduly worried if, for example, they are not good at recalling numbers. Even some healthy individuals will naturally score better or worse than their peers. But we would encourage anyone who has any concerns or notices that their memory or recall is getting worse to speak to their GP.”
Dr Rittman said the findings could also help identify people who can participate in clinical trials for potential new treatments. “The problem with clinical trials is that by necessity they often recruit patients with a diagnosis, but we know that by this point they are already some way down the road and their condition cannot be stopped. If we can find these individuals early enough, we’ll have a better chance of seeing if the drugs are effective.”
The research was funded by the Medical Research Council with support from the NIHR Cambridge Biomedical Research Centre.
Paper Reference
Swaddiwudhipong, N, et al. Pre-Diagnostic Cognitive and Functional Impairment in Multiple Sporadic Neurodegenerative Diseases. Alzheimer’s & Dementia; 13 Oct 2022; DOI: 10.1002/alz.12802
Referrals to long COVID clinic fell by 79% following roll-out of the vaccine
Referrals to Cambridge’s long COVID clinic fell dramatically in the period August 2021 to June 2022, which researchers say is likely due to the successful rollout of the vaccine.
According to the Office of National Statistics, in July this year an estimated 2 million people in the UK were living with self-reported long COVID – that is, symptoms continuing for more than four weeks after their first suspected coronavirus (COVID-19) infection. Patients report symptoms including fatigue, muscle aches, memory problems and shortness of breath more than six months post-acute COVID-19, and a significant number of patients have not fully recovered two years since the initial infection.
Two recent studies have suggested that vaccination strongly reduced long COVID symptoms one-to-three months after infection, but another study using a cohort of US Army Veterans suggested a more modest, 15% reduction at six months.
In May 2020, Addenbrooke’s Hospital, part of Cambridge University Hospitals NHS Foundation Trust (CUH), set up a long COVID clinic, with patients referred to the clinic based on a number of criteria, one of which is symptoms duration of at least five months. These patients tend to be those on the severe end of the symptom spectrum, having been referred following assessment by a team that includes a GP, mental health practitioners, physio and occupational therapists amongst other specialists.
Researchers at the Cambridge Institute of Therapeutic Immunology & Infectious Disease (CITIID) at the University of Cambridge and CUH, analysed data from the clinic and found a 79% drop in the number of patients being referred to the clinic from August 2021 to June 2022, compared to August 2020 to July 2021. The decrease began five months after people started receiving second doses of COVID-19 vaccines.
Six-month moving averages fell from around 10 referrals per month to just one or two referrals per month. This effect has so far been sustained until at least June 2022, despite four times more cases per month of acute COVID-19 in England across the same time periods.
Dr Ben Krishna from the University of Cambridge said: “Long COVID can have a significant impact on an individual’s life, and the large number of patients still experiencing symptoms many months after infection is placing additional strain on our healthcare services.
“We know that rollout of the vaccines has had a major impact on the number and severity of COVID infections, and evidence from our clinic suggests that it has also played an important role in reducing the rates of the most severe long COVID cases.”
The researchers say that it is possible – but unlikely – that the emergence of the Delta variant may also have affected long COVID rates. However, the observed reduction in long COVID rates in August 2021 was from patients experiencing symptoms for five months, which they say would suggest a change beginning in March 2021. This correlates well with the second doses of vaccination in the UK, but the Delta wave did not begin until April 2021.
The team say they also cannot rule out prior infections providing immunity that protects against long COVID from reinfections; however, primary infections were more common than reinfections around March-April 2021.
The team observed no changes in symptoms between those referred for long COVID before or after vaccination for any of the major symptoms such as fatigue (73% pre-vaccination vs 76% post vaccination) and shortness of breath (18% pre-vaccination vs 23% post-vaccination).
It is not yet clear what level of immunity is required to protect against long COVID, say the researchers. As immunity wanes over time, booster shots – including variant-specific booster shots – may be necessary to minimise long COVID risk.
Dr Nyaradzai Sithole from CUH said: “As the virus continues to circulate and infect – and in many cases, re-infect – people, it’s important that everyone is up-to-date with their vaccinations. This will not only help prevent, or at least lessen, their primary COVID infection, but should reduce their risk of long COVID. But whether with the emergence of new variants we will begin to see an uptick in the number of cases of long COVID remains to be seen.”
The study is published in Clinical Infectious Diseases.
The research as funded by the Addenbrooke’s Charitable Trust and the National Institute for Health and Care Research (NIHR), with support from the NIHR Cambridge Biomedical Research Centre.
Paper Reference
Krishna, B et al. Reduced incidence of Long COVID referrals to the Cambridge University Teaching Hospital Long COVID clinic. Clinical Infectious Diseases; 1 Aug 2022; DOI: 10.1093/cid/ciac630
Celebrating the role of patients in improving radiotherapy services
A new display in Addenbrooke’s Hospital highlights how patients have helped shape radiotherapy treatment.
The multimedia installation in the entrance to the Radiotherapy Department has been produced in partnership with a group of patients, some of whom have shared their experience of radiotherapy treatment.
In 2019 Cambridge was named by Cancer Research UK as one of seven centres of excellence in radiation research. When Rachael Webster, former Senior Radiographer at Addenbrooke’s, heard the good news, her mission was to include patients’ experience and views in the new RadNet Cambridge Centre’s plans to improve radiotherapy for future patients.
She said: “After a chat with one of our patient representatives we thought the best way to get more people involved in radiotherapy research is to celebrate the amazing work from patients and the public over many, many years that has helped shape the radiotherapy services we see today.”
The idea to develop a display about patient involvement in radiotherapy research began a year ago when Rachael put out adverts – at local events, online and via Facebook – inviting people who had experience of radiotherapy to be involved in a creative project.
Rachael soon assembled a group of nine patients and members of the public who were keen to be involved.

“Involving patients was the goal from the very beginning, we need to hear the patients’ voices to celebrate the patients’ voices,” she explained.
“There are a lot of misconceptions and fears about radiotherapy, especially from the past. We know radiotherapy is a safe, accurate and effective treatment for many cancers and around 50% of patients will received radiotherapy as a part of their treatment.”
Over the course of the year, the patient and public involvement group met with researchers, radiographers and designers to share the questions and concerns they had before they started their treatment, and to reflect on their honest experiences of undergoing radiotherapy.
People joined the group for different reasons. Neil said: “I wanted to be involved in the project so that I could help to promote the modern science of radiotherapy and how it can benefit patients.”
Beverly wanted to help others facing treatment, adding: “I feel more knowledgeable, more comfortable and I feel quite an advocate for helping people to feel the same. It was a way of giving something back that felt really important to me.”
And Caroline valued the opportunity to get involved, explaining: “Knowing that there was a way to make your voice heard and a way you can make a difference for other people was very empowering for me.”
The resulting display is based around a timeline illustrating how key advances in radiation research, patient participation in radiotherapy clinical trials and patient campaign groups have shaped the service today. Along the wall are QR codes for people to download podcasts and videos to hear more about radiotherapy techniques and the patients’ experiences.
The display also highlights pioneering radiotherapy research in Cambridge to target treatment more accurately and reduce long-term side effects that affect patients’ quality of life. A clinical trial in Cambridge of over a thousand patients proved the benefits of using a more targeted radiotherapy technique, called Intensity Modulated Radiotherapy (IMRT), for early-stage breast cancer and provided evidence to help IMRT become a standard of care.
Professor Charlotte Coles, RadNet Cambridge Lead and NIHR Cambridge BRC researcher, said: “I am thrilled to see this display showcasing the invaluable and essential contribution patients make by actively shaping as well as participating in radiotherapy research. I hope that conveying the incredible advances in radiotherapy research in such an accessible and relatable way will give patients and families added confidence in their radiotherapy and inspire them to get involved in research.”
The RadNet Cambridge team are keen to involve more patients, particularly those in under-represented groups, to share their experiences and to guide future research projects and clinical trials. Amy, one of the patients in the group, said: “My message to those who are approached to participate in a project like this, or to participate in some of these research projects, is that we need to be in it to influence it.”
The project has been funded by Addenbrooke’s Charitable Trust with additional funding and support from RadNet Cambridge and the Cancer Research UK Cambridge Centre.
Welcome to our new Patient and Public Involvement coordinator
Gail will be working with Dr Amanda Stranks, Patient and Public Involvement (PPI) Strategy Lead, to help researchers design PPI plans for their studies and run training sessions.
Gail will also be the first point of contact for our 70+ PPI panel members and will be welcoming new volunteers when they join.
Welcome Gail, tell us about yourself, what was your previous role and what do you like to do in your spare time?
I previously worked for the Ophthalmology department, as a theatre coordinator.
Prior to this, I was responsible for rebuilding both the paediatric Sleep Study and Long-Term Ventilation services for children with respiratory disorders.
I am currently studying a BA (hons) degree in English Literature and Creative Writing in my spare time.
What made you want to work in research?
The word research is derived from the Middle French ‘recherché’ which means ‘to go about seeking’. I have always been curious and I believe my fondness of research was built on this foundation.
What are you looking forward to in this role?
Learning, facilitating and possibly making a small contribution to the vast world of research.
If you need help with your Patient and Public Involvement contact the team at: cuh.ppi@nhs.net
Large number of stem cell lines carry significant DNA damage, say researchers
Cambridge researchers say detailed genetic characterisation including whole genome sequencing can help ensure safety of cell-based therapies
DNA damage caused by factors such as ultraviolet radiation affect nearly three-quarters of all stem cell lines derived from human skin cells, say Cambridge researchers, who argue that whole genome sequencing is essential for confirming if cell lines are usable.
Stem cells are a special type of cell that can be programmed to become almost any type of cell within the body. They are currently used for studies on the development of organs and even the early stages of the embryo.
Increasingly, researchers are turning to stem cells as ways of developing new treatments, known as cell-based therapies. Other potential applications include programming stem cells to grow into nerve cells to replace those lost to neurodegeneration in diseases such as Parkinson’s.
Originally, stem cells were derived from embryos, but it is now possible to derive stem cells from adult skin cells. These so-called induced pluripotent stem cells (iPSCs) have now been generated from a range of tissues, including blood, which is increasing in popularity due to its ease of derivation.
However, researchers at the University of Cambridge and Wellcome Sanger Institute have discovered a problem with stem cell lines derived from both skin cells and blood. When they examined the genomes of the stem cell lines in detail, they found that nearly three quarters carried substantial damage to their DNA that could compromise their use both in research and, crucially, in cell-based therapies. Their findings represent the largest genetic study to date of iPSCs and are published today in Nature Genetics.
DNA is made up of three billions pairs of nucleotides, molecules represented by the letters A, C, G and T. Over time, damage to our DNA, for example from ultraviolet radiation, can lead to mutations – a letter C might change to a letter T, for example. ‘Fingerprints’ left on our DNA can reveal what is responsible for this damage. As these mutations accumulate, they can have a profound effect on the function of cells and in some cases lead to tumours.
Dr Foad Rouhani from the Department of Surgery at the University of Cambridge and the Wellcome Sanger Institute said: “We noticed that some of the iPS cells that we were generating looked really different from each other, even when they were derived from the same patient and derived in the same experiment. The most striking thing was that pairs of iPS cells would have a vastly different genetic landscape – one line would have minimal damage and the other would have a level of mutations more commonly seen in tumours. One possible reason for this could be that a cell on the surface of the skin is likely to have greater exposure to sunlight than a cell below the surface and therefore eventually may lead to iPS cells with greater levels of genomic damage.”
The researchers used a common technique known as whole genome sequencing to inspect the entire DNA of stem cell lines in different cohorts, including the HipSci cohort at the Wellcome Sanger Institute and discovered that as many as 72% of the lines showed signs of major UV damage.
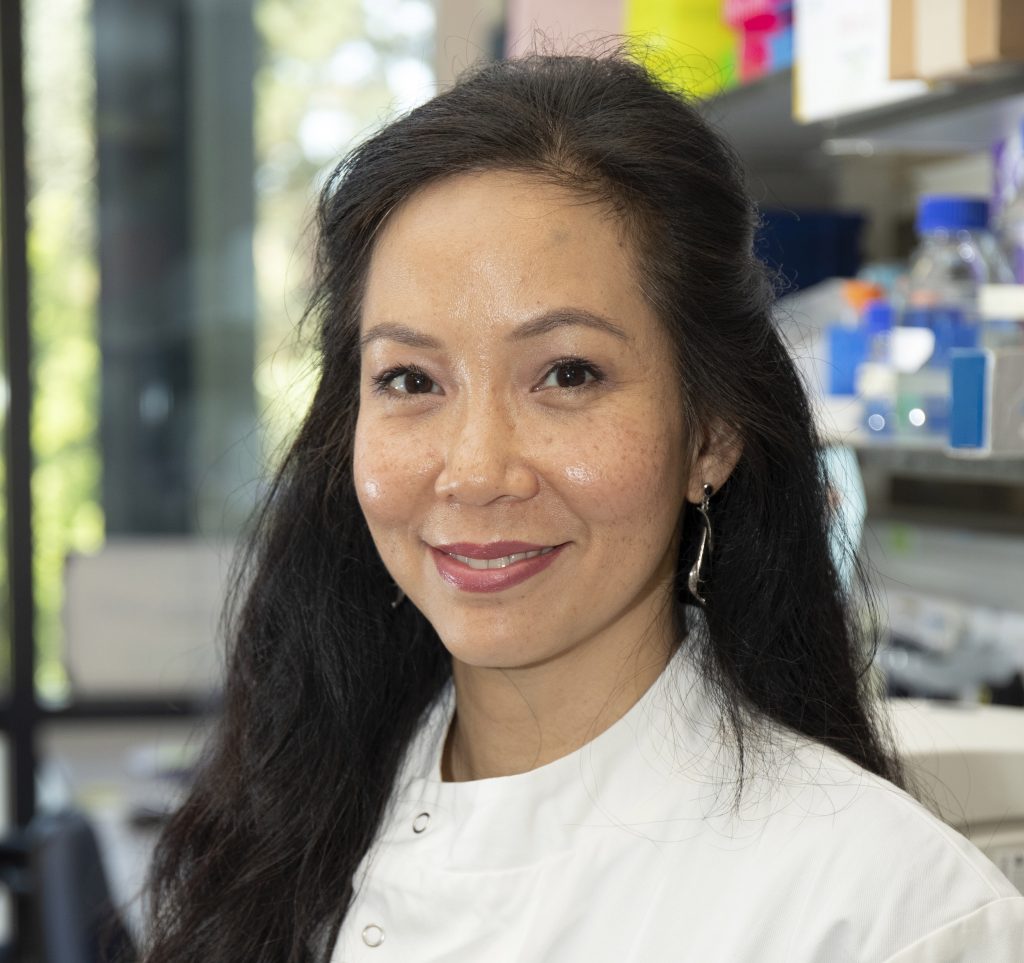
Professor Serena Nik-Zainal from the Department of Medical Genetics at the University of Cambridge, pictured right, said: “Almost three-quarters of the cell lines had UV damage. Some samples had an enormous amount of mutations – sometimes more than we find in tumours. We were all hugely surprised to learn this, given that most of these lines were derived from skin biopsies of healthy people.”
They decided to turn their attention to cell lines not derived from skin and focused on blood derived iPSCs as these are becoming increasingly popular due to the ease of obtaining blood samples. They found that while these blood-derived iPSCs, too, carried mutations, they had lower levels of mutations than skin-derived iPS cells and no UV damage. However, around a quarter carried mutations in a gene called BCOR, an important gene in blood cancers.
To investigate whether these BCOR mutations had any functional impact, they differentiated the iPSCs and turned them into neurons, tracking their progress along the way.
Dr Rouhani said: “What we saw was that there were problems in generating neurons from iPSCs that have BCOR mutations – they had a tendency to favour other cell types instead. This is a significant finding, particularly if one is intending to use those lines for neurological research.”
When they examined the blood samples, they discovered that the BCOR mutations were not present within the patient: instead, the process of culturing cells appears to increase the frequency of these mutations, which may have implications for other researchers working with cells in culture.
Scientists typically screen their cell lines for problems at the chromosomal level – for example by checking to see that the requisite 23 pairs of chromosomes are present. However, this would not be sufficiently detailed to pick up the potentially major problems that this new study has identified. Importantly, without looking in detail at the genomes of these stem cells, researchers and clinicians would be unaware of the underlying damage that is present with the cell lines they are working with.
“The DNA damage that we saw was at a nucleotide level,” says Professor Nik-Zainal. “If you think of the human genome as like a book, most researchers would check the number of chapters and be satisfied that there were none missing. But what we saw was that even with the correct number of chapters in place, lots of the words were garbled.”
Fortunately, says Professor Nik-Zainal, there is a way round the problem: using whole genome sequencing to look in detail for the errors at the outset.
“The cost of whole genome sequencing has dropped dramatically in recent years to around £500 per sample, though it’s the analysis and interpretation that’s the hardest bit. If a research question involves cell lines and cellular models, and particularly if we’re going to introduce these lines back into patients, we may have to consider sequencing the genomes of these lines to understand what we are dealing with and get a sense of whether they are suitable for use.”
Dr Rouhani adds: “In recent years we have been finding out more and more about how even our healthy cells carry many mutations and therefore it is not a realistic aim to produce stem cell lines with zero mutations. The goal should be to know as much as possible about the nature and extent of the DNA damage to make informed choices about the ultimate use of these stem cell lines.
“If a line is to be used for cell based therapies in patients for example, then we need to understand more about the implications of these mutations so that both clinicians and patients are better informed of the risks involved in the treatment.”
The research was funded by Cancer Research UK, the Medical Research Council and Wellcome, and supported by NIHR Cambridge Biomedical Research Centre and the UK Regenerative Medicine Platform.
Paper Reference
Rouhani, FJ, Zou, X, Danecek, P, et al. Substantial somatic genomic variation and selection for BCOR mutations in human induced pluripotent stem cells; Nat Gen; 11 Aug 2022; DOI: 10.1038/s41588-022-01147-3
Hundreds more to join Covid study to help protect most at risk
Up to 1,700 more patients from across the UK are being asked to join an Addenbrooke’s led drug trial, to help find ways of protecting those with poor immunity from catching Covid.
Dr Rona Smith, consultant in renal medicine at Cambridge University Hospitals NHS Foundation Trust (CUH) and senior research associate at the University of Cambridge is leading the PROTECT-V trial.
So far the trial has been testing the drug Nicolsamide on around 1,400 immunocompromised patients across 40 sites. Now hundreds more patients are needed to test a second drug, Sotrovimab, which has shown promising results for treating Covid in people at high risk of disease progression1.
If proven to be safe and effective, Sotrovimab could be considered as a preventative treatment option for Covid, for patients who are immunocompromised, either due to their disease or the treatment they are receiving for their disease.
This includes patients receiving chemotherapy for cancer treatment, immunosuppressive medications for autoimmune diseases or organ transplants, or patients with immunodeficiency.
These patient are at particularly high risk from Covid and its complications, due to a reduced ability to be able to fight the virus, leading to severe infection and hospital admission. They have also been shown to have poorer responses to vaccines than healthy individuals, and so identifying a drug that provides these vulnerable patients with protection is crucial.

Dr Rona Smith chief investigator for the PROTECT-V trial, pictured right, said:
“A preventative drug for the most at-risk in our populations could help to reduce hospital admissions, and potentially save many lives each year.”
“The launch of the Sotrovimab arm of PROTECT-V is a very exciting development. Not only does it add a second potential preventative drug to the platform, but also broadens inclusion beyond renal patient populations to any individual who has mounted a sub-optimal response to vaccination; fostering cross-specialty working to strengthen research.”
Dr Davinder Dosanjh, co-lead for the Sotrovimab arm of PROTECT-V and Deputy Clinical Director of Research at University Hospitals Birmingham NHS Foundation Trust (UHB), said:
“At UHB we have one of the largest cohorts of immunocompromised patients in the country who are not able to mount a protective immune response to vaccination, and so we have worked hard with our partners to design a trial which we believe will be of great benefit to them.”
“The trial will help us to understand the immune response to Covid in these individuals who mount sub-optimal vaccines responses, as well as investigating whether Sotrovimab provides a protective effect against infection.”
Hilary Fanning, Director of Research Development and Innovation at UHB, said:
“UHB are delighted to support this trial. This is a great example of NHS hospitals working collaboratively with academic and industry partners to deliver a clinical trial, which has direct and immediate relevance to the patients we care for. As the NHS hospital that has provided care for more patients with Covid than any other, we remain committed to contributing to the discovery of evidence-based treatments, to ensure we provide the best possible care for patients.”
UHB will be one of the key recruiting sites, alongside CUH. The Sotrovimab arm of the trial begins on Monday 8 August, with the first dose of Sotrovimab due to be administered at the Queen Elizabeth Hospital Birmingham. The first dose is due to be administered at CUH on Monday 15 August. There are plans to roll out to at least 20 other centres across the UK in the coming weeks.
Launched in Cambridge in February 2021, PROTECT-V (Prophylaxis for patients at risk of COVID-19 infection) is a platform study funded by GSK, and sponsored by University of Cambridge and Cambridge University Hospitals NHS Foundation Trust (CUH). It falls within the CUE-TIP (Covid-19 Understanding and Elimination-Trials Implementation Panel) portfolio, which includes research leading to the understanding and elimination of Covid.
The core PROTECT-V trial infrastructure is supported by grant awards from Kidney Research UK, LifeArc, the NIHR Cambridge BRC and Addenbrooke’s Charitable Trust. The Sotrovimab arm of the PROTECT-V study is funded by GSK.
1 Gupta et al (2021) New England Journal of Medicine, found an 85% relative risk reduction of progression of disease leading to hospitalisation or death, in patients treated with Sotrovimab: https://www.nejm.org/doi/full/10.1056/NEJMoa2107934
Heart surgery delays will cost lives, warns research
Urgent action is needed to clear the backlog of people with a common heart condition who are waiting for lifesaving treatment, according to research supported by the British Heart Foundation which was published in BMJ Open. The researchers have warned that a lack of action could result in thousands of people dying while waiting for treatment.
The Covid-19 pandemic has led to thousands of heart procedures being postponed and record waiting lists. Previous work has estimated that 4,989 people in England with severe aortic stenosis missed out on life saving treatment between March and November 2020.
Aortic stenosis develops when the heart’s aortic valve becomes narrowed, restricting blood flow out of the heart. Prompt treatment is vital for people diagnosed with severe aortic stenosis, as around 50 per cent will die within two years of symptoms beginning.
Now, an international team of researchers has modelled the impact that increasing treatment capacity and using a quicker, less invasive treatment option would have on waiting lists. Even in the best-case scenario, they found that the waiting list would take nearly a year to clear and over 700 people would die while waiting for treatment.
The traditional treatment for aortic stenosis involves replacing the narrowed valve, most commonly through open heart surgery (a surgical aortic valve replacement, SAVR). However, a newer keyhole procedure called a transcatheter aortic valve implantation (TAVI) is increasingly being used and is now recommended for patients aged 75 and over.
The researchers investigated the impact that increasing treatment capacity and converting a proportion of operations to the quicker TAVI procedure would have on the backlog. They looked at how long it would take to clear the backlog and the number of people who would die while waiting for treatment.
They found that the best and most achievable option involved a combination of increasing capacity by 20 per cent and converting 40 per cent of procedures from SAVR to TAVI. This would clear the backlog within 343 days with 784 deaths while people wait for treatment.
The team say they want to see greater collaboration at local and national levels to agree the changes needed that can ensure that people with severe aortic stenosis receive lifesaving treatment as quickly as possible.
Professor Mamas Mamas, Professor of Cardiology at Keele University and consultant cardiologist at University Hospitals of North Midlands NHS Trust, was one of the leading researchers in the study. He said: “Before the pandemic around 13,500 SAVR and TAVI procedures were performed each year across the UK. Increasing capacity by 20 per cent would represent one or two additional TAVI procedures each week per centre. We think that with local and national collaboration this increase is achievable. Furthermore, we have created an algorithm that NHS Trusts can use to work out the best approach locally.
“Since November 2020 the UK has been hit with further waves of Covid-19 which have led to extreme pressure on the NHS and additional delays to treatment. We expect that number of people waiting for treatment in recent months will be even higher than the figure we used in our study.
“Doing nothing is simply not an option. If we continue as we are currently thousands of people will die from untreated aortic stenosis.”
Dr Sonya Babu-Narayan, Associate Medical Director at the British Heart Foundation and consultant cardiologist, said: “We welcome the use of innovative cardiovascular procedures that can reduce the need for open heart surgery where appropriate and where their use will provide the greatest benefit to patients.
“But, as this modelling study shows, even increased use of this quicker and less invasive procedure won’t be enough to overcome the impact of Covid-19 related delays and stop people with aortic stenosis dying while waiting for treatment.
“Cardiac care can’t wait. The NHS desperately needs additional resources to help it tackle the backlog of care and ensure that heart patients receive the treatment and care they need.”
This research was part funded by the EPSRC Cambridge Centre for Mathematics of Information in Healthcare and supported by the NIHR Cambridge BRC.
New genomic testing provides vital diagnosis for severely ill babies
More than a third of severely sick babies referred for rapid whole genome sequencing receive vital genetic diagnosis in latest study across the East of England.
Results from the latest Cambridge genomic study supported by NIHR Cambridge BRC and NIHR BioResource, confirm rapid whole genome sequencing (WGS) as an effective early test to aid diagnosis in severely ill children.
WGS can determine variations in any part of the genome. By looking at all the genes in the genome it is possible to uncover disease-causing changes with a single test. This is important as some of the findings can be in unexpected genes.
Building on the findings from the Next Generations Children’s Project (2019), over 500 seriously ill children and their parents across the East of England – average age of 8.5 months – were recruited from several paediatric service settings. The aim was to provide greater insight into the benefits of rapid WGS compared to other routine genetic tests in areas such as neonatal intensive care units (NICU), paediatric intensive care units (PICU), paediatric neurology clinics and clinical genetics clinics.
Researchers worked hand in hand with scientists at East Genomic Laboratory Hub, based in Addenbrooke’s hospital, Cambridge to deliver the testing.
Findings illustrate that children in all four settings benefited from WGS testing at an early stage of their diagnoses, with patients referred from neurology having the highest percentage of confirmed diagnosis (46%), 31 % in PICU and 25% in NICU. Diagnostic rates were highest in patients with neurodevelopmental delay, hypotonia, seizures or suspected mitochondrial disorder.
In 90% of cases, both parents contributed DNA samples alongside their child in tests known as a ‘trio analysis’, which is now the gold standard test within the NHS. Comparing patient’s and parents’ DNA changes allows for identification of new information on known disease-causing genes and for the discovery of several new genes not suspected prior to testing.

Professor Lucy Raymond, Professor of Medical Genetics and Neurodevelopment at the University of Cambridge and Honorary Consultant at Cambridge University Hospitals NHS Foundation Trust, pictured right, commented: “We found that overall one in three patients received a vital diagnosis and importantly more than one in five diagnoses would have been missed without the broad analysis carried out by WGS testing. Diagnoses that were identified included spinal muscular atrophy (SMA) and other neurodegenerative conditions including some rare epilepsies, which are now eligible for precision medical therapies in the NHS.
“Finding a diagnosis changes management, stops unnecessary tests, and reassures families that everything has been done that can be done for their child.
“Rapid parent and child WGS (or trio) analysis is an excellent single test suitable for many patients as soon as possible on admission to hospital or specialist clinic. However, this must be supported by sufficient training for clinicians as well as scientific expertise for robust analysis of results.”
Many genes that can cause a rare disease have not yet been identified, so a negative result – or an unconfirmed diagnosis – does not mean a condition isn’t genetic. It does however highlight the need to keep looking at the genome to find new genes that cause disease and to help clinicians and families in the future.
Professor Raymond added: “Continuing follow-up of families within national genomic research databases such as the NIHR Bioresource or the National Genomics Research Library enables involvement in further social and health research and new genomic discoveries alongside potential recruitment to clinical trials beneficial to patients.”

Professor David Rowitch, Paediatrician (neonatology) and developmental neuroscientist and NIHR Cambridge BRC paediatric theme lead, pictured left, said: “The study highlights that the burden of genetic disorders in paediatric inpatient and specialist clinic settings is much higher than previously suspected. The finding that children in neurology have a 46% rate of diagnosis by WGS is likely to be quite surprising to many clinicians.”
“It also shows that frequent re-analysis of patient WGS data improved the diagnostic rate as new genes were confirmed and published by other sources. Moreover, by sharing data and contributing to the international rare disease endeavours, other patients can hopefully receive a potential diagnosis.”
Dr Topun Austin, Consultant Neonatologist, Neonatal Intensive Care Unit CUH commented: “The time taken to reach a diagnosis in these children can often be prolonged, requiring multiple tests and consultations. Rapid trio WGS in the NICU has enabled newborn infants with complex illness to be diagnosed at an earlier stage, which can significantly impact on their management.
“This study supports the 2019 research findings and provides further evidence of the value of rapid WGS to staff and patients. The NHS now provides rapid sequencing across all NICU and PICUs in the UK clearly showing how research can make a meaningful impact on clinical care”.
Jo Balfour, Managing Director, Cambridge Rare Disease Network commented: “It is the most worrying time for a family when their child is unwell and the reason is unknown. Whilst rapid WGS does not promise a clear diagnosis for every child with a rare health condition, research that supports advances in genomic testing to help more children and their families is welcome”.
The research was supported by the NIHR Cambridge Biomedical Research Centre, NIHR Rare Disease Bioresource, The Rosetrees Trust, and Isaac Newton Trust. Thanks also to Health Education England’s Higher Specialist Scientist Training programme which enabled East GLH staff time on this project.
Celebrating International Clinical Trials Day
On the 20 May, healthcare workers, researchers, patients and communities come together around the world to mark International Clinical Trials Day. Our research staff and patients tell us why they think clinical trials are important.
Read what they had to say below or watch these videos from our participants and research staff.

Michelle, NIHR Cambridge CRF participant said:
“I decided to join a research trial because my cancer returned and my doctors gave me two options, start chemo again or join this research trial.
The nurses have been great, putting me at ease and have looked after me. The set-up feels different here than a hospital ward. It has made me want to take part in other trials in the future.
Once you’ve joined, you feel committed and know that you’re making a real difference. Research is important because medicines won’t improve if you don’t help and take part.”

David, NIHR BioResource participant said:
“I have just taken part in a flu vaccine study and donated my last blood sample. It was really easy and straightforward.
The first study I ever took part in was for prostate cancer several years ago, and by chance, the team found cancer cells even though I had no symptoms and I was able to get it treated quickly.
That prostate study saved my life, if it wasn’t for that, I wouldn’t be here today. Research is important and we need more people to take part.”

Jennifer, NIHR BioResource participant said:
“I’m a researcher and I know how important it is to have clinical data for research, so I could not, not take part.
I took part in a COVID-19 study as a healthy volunteer and I was asked to donate some blood. I was here for 10 minutes and I was surprised how quick my appointment was. I’ve really enjoyed receiving the published articles and what the researchers found using my data. It’s exciting to be able to make a difference doing something so simple, because you never know if you or a family member may need that treatment.”

Ian, NIHR BioResource participant said:
“I have an interest in medicine and the advancements made in science. I am grateful to the NHS for all their work and have been donating blood for 55 years, so that’s why I take part in research.
My latest trial was for a flu study and I have to give several blood samples over a period of time, all the appointments have been fine.
Research is important because medicine can’t advance without it. The more people that can help means more health conditions could be resolved.”

Vera, NIHR Cambridge CRF participant said:
“I was invited to take part in a cancer trial by my doctor. I read through the notes and thought why not? If it doesn’t help me, it might help someone else in the future.
Taking part in research is really important and I am thankful for the opportunity and that we have so much research happening in Cambridge.
I would encourage anyone to take part in research if you get the chance. All the nurses are lovely and nothing is too much trouble.”

Gillian, NIHR BioResource participant said:
“I started taking part in research because a family member had health problems and I wanted to help future patients and the NHS.
My last trial was for a COVID-19 study and I was asked to donate some blood. It’s really quick and I’ve never had to wait. I donate a sample and then I can get on with my day. Everyone is really nice here.
Research is a great way to learn about diseases and it can improve healthcare. Taking part is such a small thing but it makes a big difference and it feels like you’re giving something back.”

Thea, NIHR Cambridge CRF participant said:
“My doctor suggested I join the trial and for me it felt like a last resort, but it has turned out to be more positive than I could have hoped for.
The care I have received has been wonderful, from the nurses to the study team. The study team are always happy to answer any questions I have.
I would encourage anyone to go on a trial. It’s a good routine and you always see the same people. It has been a good experience and it could help other people in the future.”

Emma, clinical research nurse, NIHR Cambridge CRF said:
“COVID-19 made me realise just how important research is and that clinical trials can be life-changing.
Working in research has been the best decision I ever made. I’m still working on a ward and providing patient care which is what I love, but I’m helping researchers find new medicines.
It’s so fulfilling, it’s more than just a job, it’s for the benefit of others. It makes a difference knowing these trials could help so many people.”

Silvana, research support assistant, NIHR Cambridge CRF said:
“I started as a cleaner at the CRF and I didn’t know then what research was. The CRF has shown me the importance of research and how it can help so many people. I see how lucky Cambridge is to have this facility.
When I became a research assistant I was given all the training I needed, learning about research and what happens during a trial. I love supporting the staff and looking after all the wonderful patients who take part.
Working here has been a great career move. It has given me so much confidence that I’m about to become a healthcare assistant and can look after more patients in the hospital.”

Erika, research sister, NIHR Cambridge CRF said:
“I’ve been in several oncology posts but working on oncology and first-in-human trials is brilliant.
The research is really fulfilling because you’re trialling something new and you’re thinking, ‘This treatment could change the future of medicine’.
There are so many highlights working in research. I see how important clinical trials are and the difference we’re making to future patients.
Our participants are amazing too, they all want to take part because they want to help others. I’ve never been a part of something so wonderful, and everyday I look forward to coming to work.”
Take Part in Research: stories from researchers and patients
This International Clinical Trials Day, find out what research means to our researchers Cathal, Zanna, Raj and Frances – and to Maureen and Wendy, who are patient participants at the NIHR Cambridge Clinical Research Facility.
Take part in a research trial with the NIHR
If you would like to take part in a research trial, find out more:
- Contact your doctor/ GP or nurse
- NIHR Be Part of Research
- NIHR BioResource
- NIHR Cambridge Clinical Research Facility
- NHS.uk
Cambridge researchers awarded Fellow status
Congratulations to our NIHR Cambridge BRC researchers who have been elected as Fellows of the Academy of Medical Sciences.
In 2022, 60 Fellows have been elected for their contributions to biomedical and health science, the highest number elected into the academy in a single year.
The Academy of Medical Sciences aims to advance biomedical and health research and its translation into benefits to society. Fellows are selected from laboratory science, clinical academic medicine, veterinary science, dentistry, medical and nursing care, and other professions allied to medical science including ethics, social science and law.

Professor Miles Parkes, director of the NIHR Cambridge BRC and one of our newly elected Fellows said: “I feel very honoured to have been elected as a fellow of the Academy of Medical Sciences and am very grateful both to the colleagues who nominated and supported my application and the many patients and collaborators across who have played a critical role in the success of our IBD research.”

Professor Fiona Gilbert, Imaging Lead at NIHR Cambridge BRC and newly awarded Fellow said: “Our work here on the Cambridge biomedical campus brings together clinical teams, research and patients, enabling pioneering working in so many fields of medicine and life science.”
Cambridge researchers elected as Fellows
Professor Miles Parkes, Consultant Gastroenterologist and Director, Addenbrooke’s Hospital NIHR Cambridge BRC director
Professor Fiona Gilbert, Head of the Department of Radiology, University of Cambridge and NIHR Cambridge BRC Imaging Theme Lead
Professor Sarah-Jayne Blakemore, Professor of Psychology and Cognitive Neuroscience, University of Cambridge, NIHR Cambridge BRC researcher
Professor David Savage, Professor of Molecular Metabolism, University of Cambridge NIHR Cambridge BRC researcher
Professor Rodrigo Floto, Professor of Respiratory Biology, University of Cambridge
Dr John Marioni, Senior Group Leader, University of Cambridge
Professor Susan Ozanne, Professor of Developmental Endocrinology, University of Cambridge
Professor Anna Philpott, Head of the School of Biological Sciences, University of Cambridge
Cognitive impairment from severe COVID-19 equivalent to 20 years of ageing, research finds
Cognitive impairment as a result of severe COVID-19 is similar to that sustained between 50 and 70 years of age and is the equivalent to losing 10 IQ points, say a team of scientists from the University of Cambridge and Imperial College London.
The findings, published today (3 May) in the journal eClinicalMedicine, emerge from the NIHR COVID-19 BioResource. The results of the study suggest the effects are still detectable more than six months after the acute illness, and that any recovery is at best gradual.
There is growing evidence that COVID-19 can cause lasting cognitive and mental health problems, with recovered patients reporting symptoms including fatigue, ‘brain fog’, problems recalling words, sleep disturbances, anxiety and even post-traumatic stress disorder (PTSD) months after infection. In the UK, a study found that around one in seven individuals surveyed reported having symptoms that included cognitive difficulties 12 weeks after a positive COVID-19 test.
While even mild cases can lead to persistent cognitive symptoms, between a third and three-quarters of hospitalised patients report still suffering cognitive symptoms three to six months later.
To explore this link in greater detail, researchers analysed data from 46 individuals who received in-hospital care, on the ward or intensive care unit, for COVID-19 at Addenbrooke’s Hospital, part of Cambridge University Hospitals NHS Foundation Trust. 16 patients were put on mechanical ventilation during their stay in hospital. All the patients were admitted between March and July 2020 and were recruited to the NIHR COVID-19 BioResource.
The individuals underwent detailed computerised cognitive tests an average of six months after their acute illness using the Cognitron platform, which measures different aspects of mental faculties such as memory, attention and reasoning. Scales measuring anxiety, depression and post-traumatic stress disorder were also assessed. Their data were compared against matched controls.
This is the first time that such rigorous assessment and comparison has been carried out in relation to the after effects of severe COVID-19.
COVID-19 survivors were less accurate and with slower response times than the matched control population – and these deficits were still detectable when the patients were following up six months later. The effects were strongest for those who required mechanical ventilation. By comparing the patients to 66,008 members of the general public, the researchers estimate that the magnitude of cognitive loss is similar on average to that sustained with 20 years ageing, between 50 and 70 years of age, and that this is equivalent to losing 10 IQ points.
Survivors scored particularly poorly on tasks such as verbal analogical reasoning, a finding that supports the commonly-reported problem of difficulty finding words. They also showed slower processing speeds, which aligns with previous observations post COVID-19 of decreased brain glucose consumption within the frontoparietal network of the brain, responsible for attention, complex problem-solving and working memory, among other functions.
Professor David Menon from the Division of Anaesthesia at the University of Cambridge, the study’s senior author, said: “Cognitive impairment is common to a wide range of neurological disorders, including dementia, and even routine ageing, but the patterns we saw – the cognitive ‘fingerprint’ of COVID-19 – was distinct from all of these.”
While it is now well established that people who have recovered from severe COVID-19 illness can have a broad spectrum of symptoms of poor mental health – depression, anxiety, post-traumatic stress, low motivation, fatigue, low mood, and disturbed sleep – the team found that acute illness severity was better at predicting the cognitive deficits.
The patients’ scores and reaction times began to improve over time, but the researchers say that any recovery in cognitive faculties was at best gradual and likely to be influenced by a number of factors including illness severity and its neurological or psychological impacts.
Professor Menon added: “We followed some patients up as late as ten months after their acute infection, so were able to see a very slow improvement. While this was not statistically significant, it is at least heading in the right direction, but it is very possible that some of these individuals will never fully recover.”
There are several factors that could cause the cognitive deficits, say the researchers. Direct viral infection is possible, but unlikely to be a major cause; instead, it is more likely that a combination of factors contribute, including inadequate oxygen or blood supply to the brain, blockage of large or small blood vessels due to clotting, and microscopic bleeds. However, emerging evidence suggests that the most important mechanism may be damage caused by the body’s own inflammatory response and immune system.
While this study looked at hospitalised cases, the team say that even those patients not sick enough to be admitted may also have tell-tale signs of mild impairment.
Professor Adam Hampshire from the Department of Brain Sciences at Imperial College London, the study’s first author, said: “Around 40,000 people have been through intensive care with COVID-19 in England alone and many more will have been very sick, but not admitted to hospital. This means there is a large number of people out there still experiencing problems with cognition many months later. We urgently need to look at what can be done to help these people.”
Professor Menon and Professor Ed Bullmore from Cambridge’s Department of Psychiatry are co-leading working groups as part of the COVID-19 Clinical Neuroscience Study (COVID-CNS) that aim to identify biomarkers that relate to neurological impairments as a result of COVID-19, and the neuroimaging changes that are associated with these.
The research was funded by the NIHR BioResource, NIHR Cambridge Biomedical Research Centre, Addenbrooke’s Charitable Trust and supported by the NIHR Cambridge Clinical Research Facility.
Paper Reference
Hampshire, A et al. Multivariate profile and acute-phase correlates of cognitive deficits in a COVID-19 hospitalised cohort. eClinicalMedicine; 28 Apr 2022; DOI: 10.1016/j.eclinm.2022.101417
New cohort created to help further research in Paediatric Inflammatory Bowel Disease
Cambridge researchers studying Inflammatory Bowel Disease (IBD) in children will now have access to a panel of young volunteers with IBD, thanks to a new research cohort from the NIHR BioResource.
The Paediatric Inflammatory Bowel Disease (PIBD) BioResource offers children and young people (0-15 years of age) living with the condition to take part in research. Researchers investigating IBD in the immune system as well as genetic or environmental factors, will be able to apply to the NIHR BioResource panel to find suitable volunteers to study the disease further and find new treatments.
Addenbrooke’s Hospital at Cambridge University Hospitals, is one of nine NHS Trusts so far in the UK that will be recruiting patients to the new arm of the NIHR BioResource. Clinicians will offer newly diagnosed IBD patients or patients already living with the disease a chance to take part in research.
Children sign up to the NIHR BioResource by providing blood, biopsy and stool samples as well as details about their health and lifestyle data, which is then anonymised and ready to be used for the purposes of research.
This new PIBD cohort led by Professor Holm Uhlig, from the University of Oxford and in collaboration with Cambridge University Hospitals and the NIHR BioResource, aims to establish a resource of more than 5,000 young patients with IBD to help researchers with their investigations and find much-needed treatments.
Treating IBD through research
Inflammatory Bowel Disease (IBD) is a term used to describe two conditions, Crohn’s disease and Ulcerative Colitis. These lifelong illnesses flare at intervals, producing debilitating symptoms including cramping abdominal pains, anaemia, weight loss and diarrhoea. They require on-going drug therapy, and many patients also require major surgery. The exact causes of Crohn’s disease and Ulcerative Colitis are unclear, but yet the number of people diagnosed with the condition is rising, especially in children.
In the UK, more than 500,000 people are affected, and despite major advances in characterising the genetic and some of the environmental factors, much work remains to be done to fully understand the disease.
It can take many years just to find the right group of patients who can participate in a particular research trial, and the aim of the NIHR BioResource is to speed up research, by bringing people and researchers together.
People can volunteer to join the NIHR BioResource by providing a blood/ saliva sample and complete a health data questionnaire. This data is then anonymised and stored securely.
When a study is accepted by the NIHR BioResource, researchers are able to select a unique cohort of samples and/or data, based on genotype (genetic makeup) and/or phenotype (a person’s traits such as age, gender, height, blood group etc.). Researchers can also invite participants to attend one of the 13 centres in England, including Cambridge, to collect more data or additional biological samples.
More than 200,000 people with and without health conditions have signed up to the NIHR BioResource and are ready to take part in research.
As well as supporting hundreds of studies, the NIHR BioResource also run their own core of research programmes within their centres in conditions such as inflammatory bowel disease, immune mediated inflammatory diseases, mental health, non-alcoholic fatty liver disease and rare genetic diseases. Adding a new cohort of people will allow researchers investigating IBD, particularly in children, to access a greater resource of volunteers and health data.
Professor Holm Uhlig, Lead Researcher for the PIBD BioResource said: “Inflammatory bowel diseases in children are increasing in numbers in the UK and worldwide. The PIBD BioResource research network provides the scientific research community with a resource of data and samples to study mechanisms of paediatric onset IBD required to develop better diagnostics and medicines.
“This collaborative project will support both UK and international research towards more personalised medicine in PIBD.”
Professor Miles Parkes, Chief Investigator for the IBD BioResource and NIHR Cambridge BRC director said: “I am delighted to see the launch of the Paediatric IBD BioResource led by Holm Uhlig and supported by key opinion leaders in paediatric IBD across the UK. There is an enormous amount to learn from studying children with IBD, of potential benefit to their future care but also impacting how we understand IBD in adults – both the similarities and the differences can be instructive.
“The opportunity to extend the highly successful IBD BioResource to support children, their families and their clinical researchers is one that we welcome, and we look forward to seeing this collaboration bear fruit in the years ahead as we research together and work towards improved treatments in IBD, and maybe one day a cure.”
Dr Nathalie Kingston, Director of the NIHR BioResource said: “NIHR BioResource is excited to be opening the Paediatric IBD BioResource with the support of our valued partners. Such a new initiative will nicely complement the recent launch of our Young People’s BioResource, which recruits young individuals through schools.
“Paediatric IBD is the first dedicated paediatric BioResource programme recruiting through NHS hospitals and Trusts, with the hope of further advancing health research in diseases appearing in both childhood and adulthood.”
First NHS Trusts who will enrol patients to the PIBD BioResource
- Oxford Children’s Hospital and University of Oxford
- Addenbrooke’s Hospital and University of Cambridge
- Alder Hey Children’s Hospital, Liverpool
- Birmingham Women’s and Children’s Hospital
- Barts and the London School of Medicine and Dentistry, London
- Royal Hospital for Children and Young People Edinburgh and University of Edinburgh
- Evelina Hospital, London
- Royal Hospital for Children Glasgow, University of Glasgow
- Great Ormond Street Hospital, London
Cambridge University Hospitals hosts one of the 13 NIHR BioResource centres, on the Cambridge Biomedical Campus, close to Addenbrooke’s Hospital. It is supported by the NIHR Cambridge BRC. You can contact the NIHR BioResource Cambridge centre team by emailing: cbr@bioresource.nihr.ac.uk or phoning: 0800 090 1212
Find out more information about the NIHR BioResource
Funding boost for ‘sponge on a string’ trial
Millions of pounds in funding has been announced for a trial that could pave the way for a ‘sponge on a string’ test to be established as a routine screening programme to detect Barrett’s oesophagus – a condition that can lead to oesophageal cancer.
Cancer Research UK and the National Institute for Health and Care Research (NIHR) are providing £6.4 million for testing of the Cytosponge-TFF3 pioneered by Professor Rebecca Fitzgerald and her team at the University of Cambridge.
The Cytosponge was created in Cambridge by Professor Fitzgerald back in 2001. Early trials were supported by the NIHR Cambridge BRC and NIHR Cambridge Clinical Research Facility, making sure the device was safe and accurate in detecting Barrett’s oesophagus.
Further studies then showed the Cytosponge detected 10 times more cases of Barrett’s oesophagus compared with routine GP care*.
The new trial, BEST4, will now explore if the Cytosponge can prevent deaths from oesophageal cancer when offered as a screening test to people on long-term medication for heartburn – one of the most common Barret’s oesophagus symptoms.
Researchers will also investigate if the Cytosponge, coupled with additional lab biomarker tests, can be used to monitor people already diagnosed with Barrett’s oesophagus instead of endoscopy, an invasive hospital procedure for which there is a major backlog caused by the pandemic.
It is anticipated the trial team will begin setting up sites in autumn, with 120,000 patients to take part over 14 years. Those involved will be randomised to different groups and a third of those will receive the Cytosponge, a quick and simple test that can be carried out by a GP.
Professor Fitzgerald will lead the trial alongside Professor Peter Sasieni and his team from King’s College London.

Professor Fitzgerald, pictured right, said: “The BEST4 trial is an exciting opportunity to take our work on the Cytosponge-TFF3 to the next level and see whether this test not only detects more cases, but also saves lives from cancer of the oesophagus. It will be a big piece of work, but it’s timely given the push from the NHS leadership, the Life Sciences Industrial Strategy and Cancer Research UK to detect cancers earlier in order to improve outcomes for patients.”
The Cytosponge begins as a pill on a string. It is swallowed by a patient and when it reaches the stomach the coating dissolves. This allows the pill to expand into a small sponge, about the size of a 50p coin. The sponge is pulled back out of the stomach by a nurse. As the sponge comes up it collects cells from the oesophagus for lab analysis.
Dr Iain Foulkes, executive director of research and innovation for Cancer Research UK, said: “Cancer Research UK is celebrating 120 years of life-saving discoveries this year and we’re really pleased to be funding what will hopefully be the final trial before this pioneering development is established as a screening device to detect Barrett’s oesophagus.
“There are 9,200 people diagnosed with oesophageal cancer in the UK every year and the Cytosponge will mean they can benefit from kinder treatment options if their cancer is caught at a much earlier stage, hopefully helping to boost survival rates at the same time.”
Using the Cytosponge during the pandemic
During the height of the pandemic patients were not being seen for routine gastroscopy. It was decided to rapidly implement use of the Cytosponge test because it has a low aerosol generation and needs only one person to carry out the procedure.
Irene Debiram-Beecham led on the implementation and at the Royal College of Nursing’s annual Nursing Awards she was highly commended in the Excellence in Cancer Research Nursing Award category. The award is sponsored by Cancer Research UK and the only one in the UK to recognise research nurses working on cancer trials and studies.
Irene, principal research nurse for the Cambridge ACED Clinic, said: “As part of this initiative, I provided a new robust training programme for nurses, clinicians and health care professionals across the UK. Having developed a system to sign them off as competent to carry out the procedure, I also provided a 24-hour support service for my colleagues if they had any questions.
“As a research nurse, it makes me proud to see something I’ve been working on for many years has finally made it into clinical practice.”
* Fitzgerald, R. C., et al. A pragmatic randomised, controlled trial of an offer of Cytosponge-TFF3 test compared with usual care to identify Barrett’s oesophagus in primary care. The Lancet, 2020
Adapted from CRUK press release
