How incurable mitochondrial diseases strike previously unaffected families
Researchers have shown for the first time how children can inherit a severe – potentially fatal – mitochondrial disease from a healthy mother. The study, led by researchers from the MRC Mitochondrial Biology Unit at the University of Cambridge, reveals that healthy people harbour mutations in their mitochondrial DNA and explains how cases of severe mitochondrial disease can appear unexpectedly in previously unaffected families.
Mitochondrial diseases caused by mutations in mitochondrial DNA are rare, affecting approximately 1 in 10,000 births, but can cause severe conditions. For example, Leigh Syndrome is a severe brain disorder causing progressive loss of mental and movement abilities, which usually becomes apparent in the first year of life and typically results in death within two to three years.
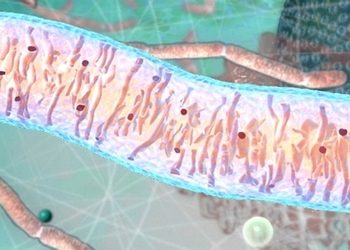
Mitochondria
Mitochondria are the powerhouses inside our cells, producing energy and carrying their own DNA instructions (separate from the DNA in the nucleus of every cell). Mitochondria are inherited from a person’s mother via the egg.
In the study, published in Nature Cell Biology, the researchers isolated mouse and human female embryonic germ cells – the cells that will go on to be egg cells in an adult woman – and tested their mitochondrial DNA.
They found that a variety of mutations were present in the mitochondrial DNA in the developing egg cells of all 12 of the human embryos studied, showing that low levels of mitochondrial DNA mutations are carried by healthy humans.
Professor Patrick Chinnery, from the MRC Mitochondrial Biology Unit and the Department of Clinical Neurosciences at the University of Cambridge, said: “We know that these devastating mitochondrial mutations can pop up in families without any previous history, but previously we didn’t know how that happened. We were surprised to find that egg cells in healthy females all carry a few defects in their mitochondrial DNA.”
For most of the human genome, mutations are kept in check by the processes of sexual reproduction, when eggs and sperm combine; however, mitochondria replicate asexually and mitochondrial DNA is inherited unchanged from the mother’s egg. This means that over time mutations can accumulate which, if left unchecked over generations, could eventually lead to malfunction and disease in offspring.
This conundrum led researchers to predict that a “bottleneck,” where only healthy mitochondria survive, may explain how mitochondria are kept healthy down the generations.
In this study, the researchers identified and measured this bottleneck for the first time in developing human egg cells. In these cells, the number of mitochondria decreased to approximately 100 mitochondria per cell, compared to around 100,000 mitochondria in a mature egg cell.
In a mature cell, a few faulty mitochondria could hide unnoticed amongst the thousands of healthy mitochondria, but the small number of mitochondria in the cell during the bottleneck means that the effects of faulty mitochondria are no longer masked.

Professor Patrick Chinnery
The exact mechanism by which cells with unhealthy mitochondria are eliminated is not yet known, but since developing egg cells need a lot of energy – produced by the mitochondria – the researchers suggest that after the bottleneck stage, eggs cells containing damaged mitochondria cannot generate enough energy to mature and are lost.
This study found every developing egg cell may carry a few faulty mitochondria, so occasionally, by chance, after the bottleneck these could be the mitochondria that repopulate the egg cell. The scientists suggest that if the quality-control step fails, then this faulty egg could survive and develop into a child with a mitochondrial disease.
Professor Patrick Chinnery said: “Unfortunately, the purification process is not perfect, and occasionally defective mitochondria leak through. This can cause a severe disease in a child, despite no one else in the family having been affected.”
Mitochondrial diseases are currently untreatable, although they can be prevented by the new technique of mitochondrial transfer – removing affected mitochondria from an egg or embryo and replacing them with healthy ones from a donor.
The study authors also suggest that this process could be relevant for human aging. Professor Chinnery added: “Previously it was assumed that the mitochondrial DNA mutations that have been associated with diseases of ageing, such as Alzheimer’s disease, Parkinson’s disease and other neurodegenerative disorders, happened over a person’s lifetime. This study shows how some of these mutations can be inherited from your mother, potentially predisposing you to late onset brain diseases.”
Professor Chinnery is a Wellcome Trust Senior Research Fellow and the researchers were funded by Wellcome, the Medical Research Council and the National Institute for Health Research.
Dr Nathan Richardson, MRC Head of Molecular and Cellular Medicine, said: “This is an exciting study that reveals important new insights into how mitochondrial diseases develop and are inherited between generations. The researchers have made great use of the tissues available from the MRC-Wellcome Human Developmental Biology Resource (HDBR). The HDBR is an internationally unique biobank resource that provides human embryonic and foetal tissue, donated through elective terminations, facilitating research into a large number of distressing medical disorders, such as mitochondrial diseases.”
The research is funded by the Wellcome Trust and the MRC with support from the NIHR Cambridge BRC.
Written by the MRC.



